Administering Social Security: Challenges Yesterday and Today
Social Security Bulletin, Vol. 70, No. 3, 2010 (released August 2010)
In 2010, the Social Security Administration (SSA) celebrates the 75th anniversary of the passage of the Social Security Act. In those 75 years, SSA has been responsible for programs providing unemployment insurance, child welfare, and supervision of credit unions, among other duties. This article focuses on the administration of the Old-Age, Survivors, and Disability Insurance program, although it also covers some of the other major programs SSA has been tasked with administering over the years—in particular, Medicare, Black Lung benefits, and Supplemental Security Income. The article depicts some of the challenges that have accompanied administering these programs and the steps that SSA has taken to meet those challenges. Whether implementing complex legislation in short timeframes or coping with natural disasters, SSA has found innovative ways to overcome problems and has evolved to meet society's changing needs.
The author is with the Office of Research, Evaluation, and Statistics, Office of Retirement and Disability Policy, Social Security Administration.
Acknowledgments: The author wishes to thank the many people in SSA who helped her locate material and those who reviewed her paper and suggested improvements. Special thanks to Susan Grad for her help and patience and to Larry DeWitt, SSA's historian, for sharing his knowledge.
Contents of this publication are not copyrighted; any items may be reprinted, but citation of the Social Security Bulletin as the source is requested. The findings and conclusions presented in the Bulletin are those of the authors and do not necessarily represent the views of the Social Security Administration.
Introduction
| ALJ | administrative law judge |
| AWR | annual wage reporting |
| BDI | Bureau of Disability Insurance |
| BDP | Bureau of Data Processing |
| BL | black lung |
| BOAI | Bureau of Old-Age Insurance |
| BOASI | Bureau of Old-Age and Survivors Insurance |
| CDR | Continuing Disability Review |
| CMS | Centers for Medicare and Medicaid Services |
| DA&A | drug addiction and alcoholism |
| DAO | Division of Accounting Operations |
| DDO | Division of Disability Operations |
| DDS | Disability Determination Services |
| DI | Disability Insurance |
| DOC | data operating center |
| DOL | Department of Labor |
| EIN | employer identification number |
| FSA | Federal Security Agency |
| FY | fiscal year |
| GAO | General Accounting Office |
| HEW | Department of Health, Education, and Welfare |
| HI | Hospital Insurance |
| IBM | International Business Machines |
| IRS | Internal Revenue Service |
| LIS | low-income subsidy |
| MCS | Modernized Claims System |
| OASDI | Old-Age, Survivors, and Disability Insurance |
| OASI | Old-Age and Survivors Insurance |
| P.L. | Public Law |
| PSC | program service center |
| RRB | Railroad Retirement Board |
| SMI | Supplementary Medical Insurance |
| SSA | Social Security Administration |
| SSI | Supplementary Security Income |
| SSN | Social Security number |
They said it couldn't be done. In 1935, the Social Security Board, predecessor of the Social Security Administration (SSA), started to plan the implementation of the Social Security Act. Board administrators contacted European experts who were experienced with such programs. The experts replied that it was impossible to maintain a system for tracking individuals' earnings histories of the scope proposed for the United States (McKinley and Frase 1970, 20–21; SSA 1997a; SSA 1964a). Despite these pessimistic assessments, the Board persevered, and the Social Security program was successfully launched 75 years ago this month—and while the agency may have stumbled a few times during its 75-year history, it is still on its feet and getting the benefit payments out via the Treasury Department every month. In fact, SSA has never missed a month of sending the payments out on time.
SSA is an efficient agency with very low administrative costs of 0.9 percent of total expenditures (Board of Trustees 2009). Agency employees have a very well-defined sense of the agency's mission, and SSA constantly strives to improve its service to the public.
Today, SSA faces many challenges. Nearly 80 million baby boomers will file for retirement benefits over the next 20 years, an average of 10,000 per day (SSA 2008e). The agency was already struggling with a backlog of disability claim hearings when the 2008 recession hit. The recession compounded the agency's problems because the number of individuals filing for retirement and disability benefits increased.1 In addition, some states furloughed the SSA-funded state employees who make disability determinations for Social Security claimants. Keeping abreast of the latest technology on a restricted budget has also been a problem. The agency is exploring solutions, such as deploying Internet-based applications that enable claimants and third-party helpers to file applications for benefits and take certain postentitlement actions themselves, freeing SSA employees for other tasks.
Nevertheless, in reviewing the SSA Annual Reports to Congress over the past 75 years, one is struck by the frequency with which the section on administering the programs starts out with a sentence such as "SSA has had a very challenging year." Reviewing some of the major challenges that SSA has faced over the years, and how SSA has met them, seems appropriate as the agency prepares to meet its current challenges.
Over the past 75 years, SSA's responsibilities have involved programs as wide-ranging as unemployment insurance, child welfare, and credit union supervision, among others. This article deals largely with administering the Old-Age, Survivors, and Disability Insurance (OASDI) program. Over the years, SSA has been tasked with administering other major programs in addition to OASDI—in particular, Medicare, Black Lung benefits, and Supplemental Security Income (SSI). This article also covers the challenges of administering those programs.
The article is not comprehensive—space constraints do not permit an exhaustive account of the many challenges the agency has faced. Also, of necessity, descriptions of legislative provisions and program policy rules are somewhat generalized. This article is meant to give the reader some sense of the scope of the programs that SSA administers and of the challenges that arise in administering such programs.
1930s
President Franklin Roosevelt signed the Social Security Act on August 14, 1935, establishing a three-person Social Security Board to administer a program of old-age retirement benefits based on a person's earnings history. The collection of payroll taxes was to begin on January 1, 1937, and the Board had to be prepared to keep records of the earnings on which those taxes were paid. So, the Board had less than 17 months to set up a recordkeeping system unparalleled in history. This would be a daunting task even if everything went smoothly, which of course it did not.
The first challenge the new agency faced was the absence of a budget. Senator Huey Long (D-LA) staged a filibuster on the closing day of the Senate session while the last deficiency appropriation bill, which included the Social Security item, was still pending. The session closed without an appropriation (Altmeyer 1966, 44). Given its deadline, the Social Security Board could not wait until the next legislative session to begin its work. The solution was to have the Federal Emergency Relief Administration,2 which had funded the President's Committee on Economic Security as a research project, set up another research project to develop ways and means of putting the Social Security Act into operation. Also, as the National Recovery Act had been declared unconstitutional in May 1935, the National Industrial Recovery Administration was liquidating and was "only too glad" to transfer office equipment and personnel to the Social Security Board (Altmeyer 1966, 44).
Building the Structure

SSA History Museum & Archives.
The original structure of Social Security operations, created in December 1935, included three operating bureaus: Public Assistance, Unemployment Compensation, and Old-Age Benefits. The Bureau of Old-Age Benefits was responsible for Title II of the Social Security Act, providing for an old-age retirement benefit. Its functions included maintaining wage records, supervising field offices, examining and approving claims, and developing actuarial estimates. There were also five service bureaus: Accounts and Audits, Business Management, Research and Statistics, General Counsel, and Informational Service (Davis 1950, 53; SSA n.d. c).
Hiring workers to supplement the staff inherited from other agencies was another challenge. The Supreme Court declared the Agricultural Adjustment Act unconstitutional on January 7, 1936, calling into question whether Social Security would survive a legal challenge and discouraging job applications. Furthermore, a civil service register of eligible applicants was not yet available. The Board made extensive use of an exception to the requirement to hire from the register—an expert and attorney exemption clause—in order to make timely hires and circumvent salary restrictions. The Civil Service Commission limited to about 100 the number of field officers who could be hired under the expert clause, and friction soon developed when the Commission started questioning the Board's proposed classifications of workers. The Board also faced pressure from Congressmen to accept political appointments. Although a few compromises were made, the Board generally held fast against hiring those deemed unqualified (McKinley and Frase 1970).
Hiring for the Bureau of Old-Age Benefits was particularly hampered; as late as March 15, 1936, the Bureau had only five employees, including the director and his assistant. By June 30, 1936, the Board had hired 677 employees for its central office in Washington and only 71 for the field. It would be December 2, 1936, before the Civil Service Commission delivered a civil service register for the Bureau of Old-Age Benefits to use (McKinley and Frase 1970).
By December 2, 1935, the Board had established a Field Organization Committee to study problems and recommend ways to establish regional and field offices of the Bureau of Old-Age Benefits (Davis 1950, 117). The Field Organization Committee recommended locations for 12 regional offices, but the Board sometimes made "capricious and unfortunate changes" either to ward off or to satisfy pressure from senators, the White House, or Board members themselves (Davis 1950, 63; McKinley and Frase 1970, 96–102). The same was true for field office locations, with Congressmen appearing before the Board to plead the cause of specific cities (Zwintscher 1952, 70). In fact, when the Board temporarily decided to cancel one Senator's home town as a field office location and also resisted hiring an unqualified protégé of his, the incensed Senator attached an amendment to the Board's 1937 appropriations limiting the salary of those hired under the Board's expert clause and cutting by 5 percent the salary of the Board executive who told the Senator "no" (McKinley and Frase 1970, 88).
In its first report of January 29, 1936, the Field Organization Committee proposed at least one "district office" per state, located in state capitals, with additional district offices based on workload. The district offices were to have primary and secondary offices (later called branch offices) under them. District offices were to report to Washington, with the Bureau's regional representative to be responsible only for inspection and training functions. However, by July 1936, the regional representatives were given full supervisory authority over all the offices in their regions (Davis 1950, 125–126).
On April 6, 1937, the Board abandoned the concept of district and branch offices in favor of "field offices," all equally under the authority of the regional representative, but varying in size and staff according to "compensable load," presumably meaning the estimated number of covered workers (Davis 1950, 126). The Board established an eight-level field-office classification system. A class I field office's compensable load was 500,000, and the office manager's salary was $5,600; a class VIII office handled a compensable load of 26,000, and the manager's salary was $2,300 (Zwintscher 1952).
In deciding on the location and geographic boundaries of the field offices, a number of factors were considered, such as convenience to the public, uniform distribution of workloads, population patterns, trading zone3 boundaries, and administrative manageability (SSA 1965, 31). The Bureau opened its first district office on October 14, 1936, in Austin, Texas. When the newly appointed manager entered the musty space on the ground floor of an abandoned post office building, the equipment consisted of some dilapidated desks and chairs left behind when the post office moved out (SSA 1960b, 26). Finding equipment for the new field offices would prove to be a continuing problem.
Each field office established "itinerant stations" (today called contact stations) in remote communities whose residents could not travel to the field office without difficulty. The field office would arrange to use free space at another agency's facility to meet with the public. Often the space would amount to little more than a desk and a chair. A field employee would visit each station on a weekly, biweekly, or monthly schedule, depending on the workload. Post offices in these locations would display posters announcing the next visit of the field office representative. As workloads increased, the Board decided it was more efficient to station representatives permanently in some of these locations than to send a representative intermittently or to convert the stations to full-fledged field offices, so it opened some of them as 1- or 2-person branch offices (equivalent to today's resident stations), with minimal records, under the supervision of the territory's field office manager (Davis 1950, 126–127; Zwintscher 1952, 95–96).
In 1937, the Bureau of Old-Age Benefits was renamed the Bureau of Old-Age Insurance (BOAI). In turn, BOAI was renamed the Bureau of Old-Age and Survivors Insurance (BOASI) when the president signed the Amendments to Title II of the Social Security Act on August 10, 1939. In 1940, the Bureau added a Control Division to handle the increased claims resulting from the 1939 amendments. Finally, BOASI established a Training Section in the Director's Office to take over the complete training program, a part of which had previously been handled by the Social Security Board (SSA n.d. c).

SSA History Museum & Archives.
Finding Office Space
Finding space for the growing agency was a major problem. The Board set up in temporary sites in Washington and split staff among multiple locations. Frequent moves and multiple locations became such a problem that Frank Bane, the Board's Executive Director, remarked that he would be quite willing to set up in a barn if he could have everyone under the same roof (McKinley and Frase 1970, 25).
It was impossible to find the kind of space in Washington that was going to be needed for the huge (and heavy) task of maintaining paper records on all Social Security number (SSN) holders and covered wage earners in the United States. Fortunately, the Board was able to find "suitable" space for its Accounting Operations close to the wharves in Baltimore—suitable more for the paper than for the employees, unfortunately. The space was in the Candler Building, a warehouse made for heavy industry that had formerly housed a Coca-Cola plant. The offices occupied by the Division of Accounting Operations (DAO) had wooden floors on top of cement, with sand in between. Employees often complained of the sand fleas (SSA 1997a). There was no air conditioning. The temperatures ranged from scorching hot in summer to freezing in winter (Simmons 1977, 12). As one Bureau employee later reported:
It was a huge factory, really. It was hot in the summer, we had the huge floor fans, which blew papers around. It didn't give us much comfort from those fans. And in the wintertime we used to sit at our cardpunch machines with our coats on and gloves because it was so cold. Then there was some company that made some kind of medication or something, the odor was horrible. They had big black bugs. I guess they came from the water. The girls used to be afraid of them, I would squash them. They made really a good sound. And another time I remember as we were sitting at our cardpunch machines, we were throwing paper clips at rats, and I mean they were rats. I remember one time the men were trying to get a rat down from the pipes that ran across the ceiling, and we watched them try to get that rat down. Then the mice, too, were doing damage, they were eating up all the data, the tabulations, etc. (SSA 1996d).
The employees worked at unfinished wooden tables whose rough lumber ran slivers into the workers' hands and arms (Altmeyer 1966, 72). Ringing bells told employees when to take their ten minute break in the morning and in the afternoon and when to go to lunch. Those wanting to smoke retired to the rest rooms to avoid sending the place up in flames (SSA 1996d). As this was during the Great Depression, people were glad to have a job even under these working conditions.
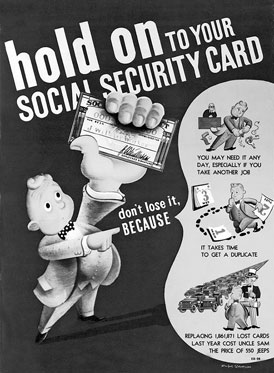
Issuing SSNs
The first step in accomplishing "the impossible" was to decide how to keep track of the earnings histories of every covered worker in the United States. A number of schemes were considered. One was a stamp system, as was used in some European countries. In this scheme, the employer would issue stamps to each employee based on the employee's earnings. The employee was to keep the stamps in a book and turn them in to the Social Security Board upon attaining age 65. In the end, however, the Board decided on the 9-digit SSN—so well known today—to identify each worker, in combination with an Employer Identification Number (EIN) to identify each employer (McKinley and Frase 1970).
The Board then had to figure out how to get an anticipated 22 million workers and 3.5 million employers registered by January 1, 1937, when the payroll tax would take effect. The plan was to set up a nationwide system of field offices to deal directly with the public, issuing numbers and taking claims; but as of September 30, 1936, the Bureau of Old-Age Benefits had only 164 employees. So, the Board turned to the Post Office Department for assistance (McKinley and Frase 1970, 309; Wyatt and Wandel 1937, 42).
The registration process was largely directed by the local postmasters. The first task was for mail carriers to make lists of employers on their routes. Their effort resulted in a list of 2.4 million employers (McKinley and Frase 1970). Beginning November 16, 1936, the post offices sent Form SS-4, Application for an EIN, to employers based on the lists they had compiled earlier that month. Along with information about the business establishment, the SS-4 asked for the number of workers employed. The mail carriers collected the completed SS-4s a week or two later. Based on the SS-4 information, the post offices delivered a supply of Forms SS-5, Application for an Account Number, to the employers the following week for distribution to employees (McKinley and Frase 1970, 368).

SSA History Museum & Archives.
Employees were permitted to return the completed SS-5 applications either to the employer, to any labor organization of which the employee was a member, to the letter carrier, or to the post office by hand or via mail (Wyatt and Wandel 1937, 54). Of the 45,000 post offices then in existence, 1,017 first class offices were designated as "typing centers" to assign the SSNs, along with 57 "central accounting" post offices to assign SSNs for the second, third, and fourth class post offices within their area (McKinley and Frase 1970, 368). The Social Security Board supplied these centers with Office Record Form OA-702, in blocks of 1,000, with the account number preprinted. For each registrant, postal employees typed the information from the SS-5 onto the prenumbered OA-702 in duplicate. The employee's name was typed onto a detachable portion of the OA-702, which was then returned to the employee—this was the Social Security card. The post office mailed the completed Social Security cards to the employer, unless the employee had brought the SS-5 to the post office and waited in person for the typed card (Wyatt and Wandel 1937).
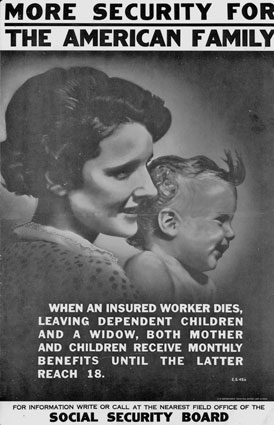
An active public information program was instituted to reach employers and employees through trade, labor, civil, veterans', and educational organizations (Pogge 1952, 5). The Board established an Informational Service in January 1936 to supervise public relations. The Board assumed that the American people would be unfamiliar with major concepts of social insurance, and the very complexity of the law necessitated a large-scale plan of popular education prior to registering employers and employees. This period coincided with the 1936 presidential campaign, and the Board was concerned about the potential for misconception and hostility toward the program (Wyatt and Wandel 1937, 30–31).
At midyear, the Informational Service prepared the publicity campaign to encourage employers and workers to complete the application forms, but they did not plan to distribute the material until after the November 3 election. However, the Board accelerated the publicity release after a September speech in which the Republican presidential candidate, Alf Landon, criticized the program in a manner the Board considered seriously misleading. Also that year, many employers, in conjunction with the Landon campaign, began stuffing payroll envelopes with leaflets designed to undermine support for the nascent program. The Social Security Board was so alarmed that Chairman John G. Winant—a top Republican politician—resigned in order to campaign in defense of the Social Security Act. In addition, in October 1936 the Board released a film called "We the People and Social Security" along with a 4-page pamphlet entitled "Security in Your Old Age." It is estimated that some 4 million people saw the film, and nearly 8 million of the pamphlets were distributed by Election Day (McKinley and Frase 1970, 357–358).
On November 6, the campaign to encourage employers and employees to register began. A series of press releases outlined the procedure for assigning SSNs and carried sample Forms SS-4 and SS-5, as well as a Social Security card specimen. The campaign included three releases on old-age benefits in 24 languages distributed to the country's foreign language press. The Associated Press, the United Press, the Hearst newspaper chain, and many individual papers ran series of articles on old-age benefits and registration for weeks at a time. During the November and December initial registration period, there were also 12 nationwide radio broadcasts by well-known individuals and a host of local broadcasts arranged by the 56 skeletal field offices then in place. Over 3 million posters were distributed, 50 million more pamphlets were dispersed, and three additional newsreel trailers were shown to some 42 million people (McKinley and Frase 1970, 364–366). In addition, the Informational Service enlisted the help of thousands of kids from the National Youth Administration to "go out to the hedgerows and by ways, the gates of feebly stirring industrial plants, business offices, and billboards" to post some 3 million placards (Swift 1960, 11).
The publicity campaign and the Post Office Department's efforts produced over 22 million completed applications as of December 22, 1936, 28 days after the initial distribution of employee applications (Wyatt and Wandel 1937, 62). During the first 4 months of the registration campaign, nearly 26 million SSNs and more than 2.6 million EINs were assigned (Corson 1938, 3). By June 1937, the Bureau had received about 30.3 million applications for SSNs (Pogge 1952, 5).
In November 1936 the Board assigned headquarters staff to 56 Bureau field offices, covering all but one of the cities where the Post Office Department had set up its "central accounting" offices. These 56 Bureau offices primarily answered questions and directed applicants to the post offices (McKinley and Frase 1970), but they were also busy working out procedures and methods with the Post Office Department and the Bureau of Internal Revenue. The field employees made extensive employer contacts—as many as 50 in a single day by some accounts. Phones rang all day with questions (SSA 1952b).
The Board twice had to ask the Post Office Department to extend its handling of the SSN applications, first through March 1937 and then through June 1937, before the Bureau could take over. During this time, Bureau employees often were stationed in the post offices to assist with typing the SSN applications (SSA 1952b). Effective July 1937, Bureau field offices—still numbering only 175 with 1,702 total employees—finally took over the enumeration workload from the post offices (Zwintscher 1952, 90; SSA 1965, 25). By that time, some 35 million SSNs had been issued at a cost of $5.7 million (SSA 1990, 1; McKinley and Frase 1970, 372). Still, the job was not finished. In July 1937 alone, Bureau field offices issued some 1.9 million additional SSNs (McKinley and Frase 1970, 368–373). Even with field office employees working evenings and Saturdays and with "managers and assistant managers, anyone who was available, pounding away at typewriters," the Bureau had to set up additional typing centers in its 12 regional offices to help with the workload (SSA 1965, 32; SSA 1952b).
Maintaining the SSNs
The post offices, and subsequently the Bureau's field offices, sent the completed SS-5 and the corresponding OA-702 forms in blocks of 500 to the Bureau's Records Office in Baltimore's Candler Building, where the SSN master files were to be kept. The local offices kept carbon copies of the OA-702 to use should an individual request a replacement card (Wyatt and Wandel 1937, 58).
The Baltimore DAO officially opened on November 9, 1936, with 18 employees. It was vital to staff the office immediately. At the time, a hiring "apportionment" was in effect that required the Bureau to recruit a certain proportion of employees from each state. As a result, employees came from all parts of the country. It was thought that the central operation in the Candler building was temporary, and that the work would soon be dispersed to the 12 regions, so recruitment from distant states was logical (SSA 1952b). However, actual operations would reveal that decentralization was not really feasible.
The personnel office received 20 applications for every person hired. Because this was during the Great Depression, applicants for what were basically clerical jobs sometimes had amazing qualifications, including many PhDs and Phi Beta Kappas. On a single day—December 7, 1936—some 940 employees entered on duty. That morning the new arrivals lined down the stairways and out around the building. As each hire had to complete three or four copies of the personnel forms, it took until 5 a.m. to process them all. The personnel office was "a three-ring circus"—operating with one thin book of rules, regulations, and instructions, officers just learned as they went along (SSA 1952b; SSA 1960a, 32).
In November and December 1936, thousands of mail bags containing the completed forms OA-702 and SS-5 began arriving at the Candler Building to be coded and checked for accuracy. Here the Bureau installed a "great battery" of International Business Machines (IBM) equipment and deployed over 2,300 machine workers and checkers to handle the applications as quickly as they came in (McKinley and Frase 1970). The Baltimore Records Office used a nine-step process to create a permanent master record and to establish an earnings record for each individual. One hundred applications and office record cards, numbered consecutively, were sent through each operation together with a control unit of nine cards (one for each step). The appropriate control card was removed at the end of a step and sent to a control file to track the status of each block (McKinley and Frase 1970, 375).
When the Records Office received the Form SS-5 and the accompanying OA-702 from the local offices, different clerks working independently converted the two sets of information into numerical codes that could be transferred to punch cards. The first group of employees keyed information from the SS-5 into a master punch card for each individual. A tabulating machine used this master punch card to set up a numerical register of accounts stored in huge loose-leaf books. These volumes contained the SSN, name, and date of birth of each number holder. Each page contained 100 SSNs in numerical order. From these volumes, employees could learn the name and identifying information of an SSN's owner in a fraction of the time that would be required to locate the master punch card (Wyatt and Wandel 1937, 120–121). The master punch card was also used in the earnings-posting operation to establish an earnings ledger for each individual.
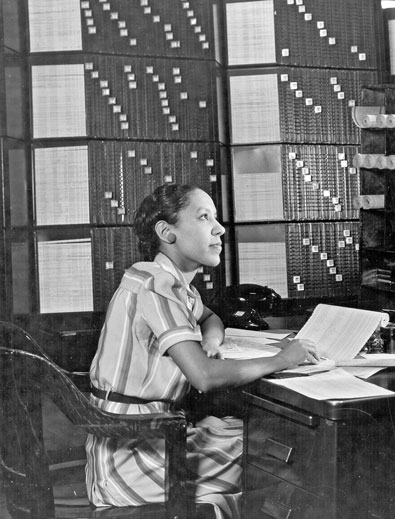
SSA History Museum & Archives.
A second group of employees independently keyed the same information coded from the OA-702 to create an actuarial punch card (Fay and Wasserman 1938, 25). The actuarial punch card was created for actuarial and statistical purposes and was also used to set up the "visible index." Later known as the National Employee Index Flexoline File, or simply Flexoline, the visible index consisted of strips of thin bamboo covered with paper, 3/16 of an inch wide by 9 inches long—one for each SSN issued—set in a steel panel. The strips were inserted into the frame one by one, with some employees filing as many as 300 strips an hour. Each strip began with a 3-digit entry based on the Russell Soundex System (in which all surnames having the same basic consonants are grouped together), followed by the individual's surname, given name, middle initial, and SSN. The strips were mechanically prepared from the actuarial punch card and manually posted on the panel, sorted by the first letter of the surname and within each letter by phonetic code, then in each code group by the first seven letters of the first name, middle initial, year and month of birth, and SSN. Up to 1,600 panels were then hung on each rack (Staruch 1978, 29). Reportedly, experienced clerks were able to find any name and its corresponding account number in less than 60 seconds. In addition, the SS-5s were filmed on 16 millimeter, noninflammable film strips. In June 1938, officials bragged "This film is so compact that the entire file of 40 million photographed SS-5s is stored in 10 ordinary letter-size file cabinets" (Fay and Wasserman 1938, 25).
Keeping all these records was a huge storage problem. Before very long, it was necessary to stack the filing cabinets in two levels, with employees using rolling ladders to look into the upper bank (SSA 1997a). By September 28, 1951, the Flexoline contained over 129 million strips and was projected to increase at the rate of approximately 5 million per year. The index occupied approximately 36,000 square feet of floor space, one city block long on one side of the floor and one-third block long on each end of the floor (SSA 1952a).
Keeping Wage Records
The Bureau used a punch card technology that was relatively simple compared with today's computer capabilities, but in the 1930s much of the machinery SSA used was truly innovative. Keeping a record of each individual's lifetime earnings was an unprecedented task, and the technology to support this Herculean effort did not even exist—the Board had to work with private industry to create the needed technology (OTA 1986, 94).
Punch cards were a little longer and narrower than postcards, and about the same stiffness. The relative position of holes punched in a card represented numbers and letters. After punching, the cards were sent through a series of special machines that used electrical circuits to permit sorting in any desired order, producing duplicates, printing the information represented by the punched holes, tabulating or summarizing the information, and checking duplicate cards to ascertain that they matched the originals (Wyatt and Wandel 1937, 119).
DAO prepared a punch card showing the employee's name, SSN, and the amount of earnings on the basis of each quarterly report. This card was checked against the corresponding master card to make certain that the name and SSN matched. If they matched, the card was run through an alphabetic accounting machine with the ledger sheet of the same individual. The machine read the amount represented by the punched holes and printed this amount on the ledger. Once a year, the quarterly earning cards for each employee were summarized to one card via a tabulator with a punch attachment, and the summary annual wage information was posted to the ledger account (Wyatt and Wandel 1937, 123).
The Board had to decide whether its records should be centralized in a single location. An expert hired by the Board strongly recommended that the records be kept in the 12 regional offices, but Bureau executives questioned the wisdom of that approach. A compromise was reached: A pilot project kept all the records in Baltimore's Candler Building, but broke them into 12 sets based on the regional designations. It was soon evident that the regional approach would not work. Workers continuously migrated from one part of the country to another, and large employers paid their taxes and filed wage reports centrally for employees all over the country. Regionally maintained records would have required a continual workload transferring volumes of records between regions and maintaining special controls to keep track of the transfers. Therefore, early in 1939, a central mechanized section was set up to maintain all wage records. Subsequently, all the related files and records were combined and centralized (Altmeyer 1966, 86).
By 1938, DAO had about 500 employees using 222 card punch machines and 70 card sorters. Each day, DAO recorded about 715,000 accounts, with each card-punch operator keying in some 2,000 workers' wage reports (SSA 1992b, 15). By 1940, the Bureau had also implemented a system for posting employee accounts on a cyclical basis so that a continuous process used a relatively stable number of employees and equipment (Pogge 1952, 5–6). The Bureau's cost of maintaining a worker's account was only about 20 cents a year (Altmeyer 1966, 87).
An early crisis took form as the "John Doe" problem. Many employers reported earnings without providing a worker's name or SSN. The first report from the Bureau of Internal Revenue did not contain SSNs for about 12 percent of the wage items—and this rapidly increased in subsequent reports. The BOAI dubbed reports without SSNs "John Does" (Altmeyer 1966, 123). The Bureau quickly established procedures to contact employers for the identification information, and the "John Doe" rate decreased substantially, to 2.5 percent as early as 1939 (Pogge 1952, 5). A series of articles by Drew Pearson, a muckraking journalist of the period, repeatedly raised alarms about the John Doe problem and eroded some public confidence in the program (SSA 1967a; Altmeyer 1966, 123). However, by the time the Pearson articles were published, SSA figures showed that John Does were less than 1 percent of total wage reports, suggesting the articles reflected political differences rather than administrative inefficiency (OTA 1986, 95). Nevertheless, the Bureau would continue to receive incorrect names or SSNs on employer wage reports, and determining the correct identification information—and educating employers about the importance of supplying correct information—remained a large task into the 1950s (Pogge 1952, 5).
The Bureau also had to deal with "delinquent employers" who failed to report their worker's wages. Field offices would check the yellow pages in the telephone directory and the city directory against EIN files in an effort to find employers who were not reporting (SSA 1955a). The offices also got lists of employers to contact from state unemployment offices (SSA 1975b).
Processing Lump-Sum Claims
In addition to making certain every covered worker had an SSN and every employer had an EIN, the Social Security Board had to determine policy and procedures for processing claims. Monthly old-age benefits were not scheduled to begin until January 1942, but workers who turned age 65 before that date—or the survivors or estates of deceased workers—were able to claim a one-time payout in lieu of monthly benefits. The Board's General Counsel also interpreted Section 205 of the Social Security Act as requiring the Board to act as the administrator for the estates of persons whose death payments would amount to less than $500. In some states, this might entail finding and paying off any creditors before paying relatives (McKinley and Frase 1970, 310–311). One former SSA Dallas Regional Commissioner recalled how complex Louisiana inheritance laws were and how tedious it was to find 15 to 20 relatives entitled to a share of lump-sum payments, frequently as small as $1 (SSA 1985b, 16).
The earliest a lump-sum payment claim could be filed was January 1, 1937, but the Board did not have the forms ready until February 5, after the procedures had been reviewed by the Comptroller General (McKinley and Frase 1970). Once they received the approved procedures, field personnel were not happy with complicated and expensive requirements, such as notarizing certain information, and feared a negative public reaction (Wyatt and Wandel 1937, 132).
At first, it was uncertain whether the claims clerks (today called claims representatives) could assist applicants. The General Accounting Office (GAO) took the position that a long-standing federal statute prohibited federal officials from assisting citizens in the prosecution of claims against the government. However, the Board argued that in this case the claimant had a statutory right to a specific benefit based on contributions into the old-age insurance system. Therefore, these were of a different character than usual claims against the government, which were payable out of general revenues. GAO relented, deciding that "it was not required to object." Once its role was settled, the Bureau impressed on its employees the importance of assisting claimants with their applications to make certain they received the benefits to which they were entitled and understood their rights and duties (Altmeyer 1966, 55). Some field office employees actively tracked down workers who had turned age 65 to notify them of their eligibility to claim benefits. Some even contacted funeral homes for information to help obtain claims for those who died after January 1, 1937 (SSA 1975b).
The manager of a local Bureau field office reviewed the claims forms and substantiating evidence (such as proof of age if the date of birth differed from that in Board records), affixed a transmittal form, and then forwarded the claims by way of the regional office to the Director of BOAI. The Director immediately transferred the forms to the Adjudication Operations Section of the Technical and Control Division. At the same time, the field office claims clerk sent a request to Baltimore's DAO to send earnings information to the Washington adjudication office (SSA 1974a). In the Washington office, a grade 5 employee in one of the four geographically based claims control units would associate the earnings information with the claim. If needed, additional information was requested from the field office. When he or she had everything needed, the employee would decide to allow or disallow the claim. The material would then go to a grade 7 reviewer who examined the claim and its substantiating evidence, determined the amount of the benefit, certified the approved claim for payment to the Treasury Department, and sent the claimant a notice (SSA 1974a).
Instructional material for processing claims was developed as work progressed. The original Social Security Act was less than six pages long, and the Board had to supplement the act with many rules and procedures for conducting its business. The first instruction on claims policy was Social Security Board Administrative Order No. 24. It included a page-and-a-half, single-spaced list of general principles for taking applications and ensuring confidentiality (McKinley and Frase 1970, 378).
The first claim was filed by a Cleveland motorman named Ernest Ackerman, who retired 1 day after the Social Security program began. During his 1 day of work under the program, his employer withheld a nickel in payroll taxes from Ackerman's pay. Ackerman received a lump-sum payment of 17 cents. During this period, the average payment was $58.06, and the smallest payment was 5 cents (SSA 1995a, 8).
In 1937 alone, the Bureau received between 70,000 and 80,000 claims for lump-sum benefits (Pogge 1952, 5; Altmeyer 1966, 86). At one point, the claims in Washington were "piled on top of file cabinets 3 feet deep." However, the Bureau soon dug itself out, and was able to assure the 1939 Advisory Council that it could handle the workload associated with moving the date when insured workers could begin receiving monthly benefits forward from 1942 to January 1, 1940 (SSA 1967a).
Training Employees
SSA's first Commissioner, Arthur Altmeyer, identified training as one of the keys to setting up a highly efficient administration in a very short time. Pervading all the training was an effort to instill in each employee his or her "affirmative responsibility for carrying out the provision of the Social Security Act" (Altmeyer 1966, 53).
The first training efforts were made as early as March 1936 when appointments to the field began. The Bureau of Research and Statistics, aided by the Field Organization Committee, improvised the initial training activities. The offices of the several Bureaus, and social insurance authorities outside the Board, conducted the training. The training generally had two components.
A 2-week basic training course emphasized the general economic background of the act. An analysis of the act's various provisions was provided for all employees above a certain grade (Wyatt and Wandel 1937, 26–27). Field staff had to be experts not only on the old-age benefits program but also on other aspects of the act, as the public had difficulty differentiating between the various parts of the program. After classes, the students' evenings in the hotel room were filled with homework and study (SSA 1965, 32).
BOAI supplemented the basic course with a 3-week technical course for its own personnel. This course stressed the Bureau's operating procedures for tasks such as keeping wage records, adjudicating benefit claims, and assigning SSNs, as well as practical details of office management, personnel, and procurement regulations. BOAI provided special after-hours instruction for lower-grade employees and for those who had originally been unable to take the basic training course. By 1937, a full-time training staff was in place, and the Board integrated all of its training activities in a special training division within the Bureau of Business Management (Wyatt and Wandel 1937, 26–27).
Early Social Security Board employees later recalled their training experience with enthusiasm. They credit this early training with imbuing employees, from top executives to clericals, with a fierce loyalty to the Social Security program and a belief in the social philosophy it represented. They absorbed the lesson that they were working for the people who paid into the Social Security trust funds, and that these people deserved their courtesy, attention, and concern (SSA 1975a).
The Board put great stock in the importance of training and devoted considerable funds to the process, but this did not translate into money for the employees, who were expected to pay for their transportation to Washington and be reimbursed later. The Board paid neither a salary check nor a per diem for the training period (SSA 1975b).
1940s
Viewing Social Security strictly from a program perspective, one might conclude that not much happened during the 1940s. However, from an administrative standpoint, it was a very active decade, starting with implementing the 1939 Amendments to the Social Security Act. Also in 1939, the President's Reorganization Plan Number 1 established the Federal Security Agency (FSA). The Social Security Board became a part of FSA and was no longer an independent agency. The FSA encompassed the Social Security Board, the Public Health Service, the Office of Education, the Civilian Conservation Corps, and the U.S. Employment Service. The objective was to bring together agencies whose major purposes were to "promote social and economic security, educational opportunity, and the health of the citizens of the Nation" (FSA 1948, v).
The process of issuing SSNs and establishing earnings histories continued apace. By the end of January 1940, DAO had established almost 49.6 million worker accounts, plus more than 1.8 million Railroad Retirement Board (RRB) employee account numbers. By April 1940, the wage records kept in Baltimore had been converted from a regional to a national basis—a transition that required 28 months to complete. By July 1940, Bureau personnel totaled 8,744, with about half in DAO, about 3,000 in the field, and the rest in D.C. (SSA 1950).
SSA History Museum & Archives.
Implementing the 1939 Amendments
Signed into law on August 10, the 1939 amendments advanced the start date for monthly benefits from January 1942 to January 1940 and added benefits for dependents and survivors of retired beneficiaries. The Bureau, now renamed the Bureau of Old Age and Survivor's Insurance (BOASI), took immediate action, mailing letters to all individuals who had filed for the lump-sum payment at age 65 to alert them to their potential eligibility for monthly benefits. DAO sent transcripts of wage records for workers who attained age 65 from 1937 through 1940 to servicing field offices to enable staff to advise claimants of their possible benefits (Pogge 1952, 6). By April 1940, 63 more field offices were opened, including some 1-person branch offices (today known as resident stations), bringing the total number of field offices to 460. In addition, 1,296 itinerant stations (today known as contact stations) were established to assist the field offices (SSA 1965, 33).
The 1939 amendments markedly changed the nature of the field offices' functions. In addition to issuing SSNs and contacting employers about wage filings, they now served large numbers of people arriving to file claims for monthly benefits. To reflect the changing nature of the job, claims clerks were renamed claims assistants (SSA 1965, 32). Even so, the field offices still only completed the applications and gathered documentary evidence; before September 1941, they did not formally determine whether benefits were payable.
In the first year of administering monthly benefits, BOASI awarded benefits to about 250,000 individuals. On January 31, 1940, Ida M. Fuller became the first person to receive an old-age monthly benefit check, in the amount of $22.54. She had paid $24.75 in Social Security taxes between 1937 and 1939 on an income of $2,484 (SSA n.d. b). By the end of 1941, a total of 372,300 benefits totaling about $6.8 million in monthly payments were in force (Pogge 1952, 6–7). The numbers may not seem high, but they signify enormous effort in the era before electronic processing devices (Altmeyer 1966, 119). These claims brought with them many policy and procedural issues to resolve, such as when a widow has a child in her care, and whether tips and traveling expenses are "wages" under the act. BOASI also had to negotiate with the Bureau of Internal Revenue on definitions. For instance, there was a large "twilight" area in which it was difficult to determine whether a worker was an employee under the act. There were no precedents to follow, and complete information with which to resolve questions was lacking.
Eventually, as experience accumulated, BOASI developed its Claims Manual of operating instructions for making entitlement determinations and processing claims (Pogge 1952, 6). The first Claims Manual was a slim 35 pages. The Bureau had so much trouble getting the manual printed that a mimeographed version was sent out in advance (Davis 1950, 221). It was April 1940 before the printed version arrived (SSA 1950). The Claims Manual outlined standards and procedures for the development, review, and adjudication of claims. It was not updated very often, so it was supplemented with "adjudication instructions," copies of which were kept by each claims adjudicator.
A policy group in the Claims Division had written the Claims Manual, but legal interpretations were largely made on the fly as cases came up. The claims adjudicators in Washington referred any case with questions about legal interpretations to the unit chief, who would take the case to the head of the Claims Division. The question would then be submitted to the General Counsel for legal opinion. Before long, claims adjudicators all had piles of different kinds of cases on their desks awaiting legal decisions (SSA 1974a).
Administering monthly benefit payments brought the problem of how best to maintain payment records. At the time, the normal accounting practice was to keep a ledger account for each individual. BOASI considered this approach, and even ordered millions of ledgers and posted payments to them for a few months, but it soon was obvious that an unacceptable number of clerks would be required to maintain the individual accounts as the benefit rolls grew. Instead, BOASI determined to use a claims folder system, with a folder set up for each account. All actions affecting payments were filed systematically in the claims folder. BOASI employees could reconstruct the payment history of any beneficiary in a matter of minutes using the claims folder (Pogge 1952, 7).
The Claims Correspondence and Control Section (later known as the Control Division) was responsible for keeping the records. The Section started off with 50 people and was budgeted to increase to 140 with the next fiscal year (FY), but it soon became apparent that over 500 employees would be needed (SSA 1952b).
BOASI also had to devise a way to make available at all times information on which persons were entitled to benefits and which were due a payment each month. The wage records operation also had to find a way to identify any beneficiaries who earned more than $14.99 per month, making them ineligible for a payment for that month. BOASI developed a punch card system for controlling the payment status of each beneficiary for each month. This system enabled the Bureau to prepare a monthly statement showing the activity of the beneficiary rolls and to balance this statement against external controls established by the Treasury disbursing office within a few days of the end of the month (Pogge 1952, 6–7; SSA 1952b).
Supporting the War Effort
No sooner was the Social Security Board's organization in place and its employees trained than another challenge arose. World War II became the nation's priority, and large numbers of BOASI employees left to join the war effort. Because agencies dealing directly with the war were given priority on hiring, finding replacements for the departing BOASI workers was problematic. The surplus of laborers during the Depression now became a shortage.
Despite its manpower challenges, BOASI supported the war effort in a number of ways. The U.S. government commissioned economic surveys to provide a base for integrating all the nation's industries into the war effort. With its widespread network of offices and its 3,900 experienced field staff, BOASI took responsibility for conducting the economic surveys. Field assistants (later renamed field representatives) had vast experience visiting employers to resolve wage-reporting problems and determine employer-employee relationships. These BOASI employees were ideal for collecting information on workers' job duties, the materials they used, the supplies they needed, and whether they had more of certain critical materials (such as steel) than they needed. The surveys went on through the spring, summer, and fall of 1942, and the information was submitted to the War Production Board (Olcott 1981, 14–15; SSA 1975b). The Bureau also provided war agencies with statistical data derived from its wage record operations (Pogge 1952, 8).
Also starting in 1942, BOASI took on a "Civilian War Benefits" program that paid benefits to families of civilian war casualties such as American construction workers in the Pacific islands. Monthly benefits for wives (and a few widows and parents) ranged between $30 and $45 depending on the worker's former wages, with children receiving less. The first payments went out in March 1942, and by December 1942 BOASI was paying $38,800 a month to 1,467 beneficiaries. This program gave BOASI its first experience handling disability-based benefits. Starting in November 1942, payment went to civilians injured while engaged in civil defense work, such as Civil Air Patrol or the Aircraft Warning Service, or during enemy actions such as the Pearl Harbor attack (Olcott 1981, 14–15). The program also paid benefits to Philippine Island civilians disabled as a result of enemy action (Pogge 1952, 8). Monthly cash benefits ranging from $10 to $85 were paid for temporary total disability or permanent disability of at least 30 percent (Altmeyer 1966, 140; DeWitt 1997). BOASI worked with physicians on loan from the Public Health Service to develop procedures and policies (SSA 1996c).
SSA History Museum & Archives.
The demand for defense-related office space in the Washington, D.C., area peaked just as a new building intended to house and centralize Social Security's headquarters was completed. BOASI had to go elsewhere. Headquarters staff moved from D.C. to Baltimore on June 1, 1942. The Claims Division and the Control Division, which respectively authorized claims payments and maintained the beneficiary records, were simultaneously merged into a Claims Control Division and decentralized from the D.C. area, moving into "area offices" in Philadelphia, New York, Chicago, San Francisco, and New Orleans (Olcott 1981, 15–16). In 1946, the New Orleans area office was moved to Birmingham, and a sixth area office was opened in Kansas City (SSA 1952b; Davis 1950, 127). The Bureau also set up a DAO branch in Wilkes-Barre, Pennsylvania (Pogge 1952, 8; SSA 1952b).
On September 15, 1941, responsibility for reconciliation of wages, development of claims, and computation of benefit amounts was shifted from the Washington Claims Division to the field offices. However, claims still received a 100-percent review and payment authorization in the Claims Division (SSA n.d. b).
BOASI also looked for ways to eliminate unnecessary work to alleviate the staffing shortage. BOASI used a special technique known as the "Why survey," in which all Bureau employees participated over several months. In this survey, the Bureau used teams of employees to analyze each operating step that had to be performed and asked "Why do we do this? Why do we do it this way? Why can't it be eliminated? Why can't it be improved? Why can't it be combined with other operations? What does this step add to the final product?" The Bureau received about 6,600 suggestions from about 2,400 employees, and adopted about a quarter of the suggestions. This effort enabled the Bureau to cope with a staff reduction from about 9,850 to 8,300 even though the workload did not decline (Pogge 1952, 8; Futterman 1960, 20).
Restructuring in the Post-War Period
On July 16, 1946, the Social Security Board was abolished. In its place, the FSA created the Social Security Administration (SSA), with all of the duties, powers, and functions of the old Board. The old Executive Director's Office became the Office of the Commissioner of Social Security. Arthur Altmeyer, who had been the Board's chairman, became SSA's first Commissioner.
There were now four "operating" bureaus (actually program bureaus): The Bureau of Public Assistance, the Bureau of Employment Security, a new Children's Bureau, and BOASI. In 1947, BOASI supervised the 12 regional representatives and their staffs, 464 field offices, 6 branch offices, 2,052 itinerant stations, and 13 detached field stations (Davis 1950; FSA 1948).
Major changes occurred in DAO. The old individual ledger sheets that held individuals' earnings histories were replaced by yearly listings prepared by an electrical accounting machine using the annual summary and detail earnings punch cards. In addition, DAO began microfilming records, which not only introduced workyear savings, but also freed up filing equipment and space. Also at this time, responsibility for assigning employer account numbers was transferred to the Bureau of Internal Revenue (Pogge 1952, 9).
1950s
The 1950s were a period of growth for SSA, in coverage of additional workers, in new beneficiary entitlements, and in agency employment. While taking on new workloads, SSA also had to deal with inadequate and substandard facilities.
The decade brought many structural changes for SSA. By 1952, there were over 500 field offices (SSA 1952b). On July 19, 1954, the field offices were redesignated "district offices," although the agency has since continued to refer to both district and branch offices generically as field offices. Area offices were renamed "payment centers" on July 8, 1958. In September 1958, a new payment center was established in Baltimore to handle cash disability payments and the Old-Age and Survivors Insurance (OASI) payments for beneficiaries living in foreign countries (SSA n.d. b).
Meanwhile, SSA became a part of a new agency. On April 11, 1953, President Dwight Eisenhower abolished the FSA and in its place created the Department of Health, Education, and Welfare (HEW).
Implementing the 1950 Amendments
The 1950 Social Security Act Amendments extended coverage under the OASI program to about 10 million more persons effective 1951, including the nonfarm self-employed other than doctors, lawyers, engineers, and members of certain other professional groups; regularly employed domestic and farm workers; a small number of federal employees who were not covered under the civil service retirement program; members of a few very small occupational groups; and workers in Puerto Rico and the Virgin Islands. In addition, voluntary coverage was offered to the 1.5 million people who worked for state and local governments but were not under retirement systems and to about 600,000 employees of nonprofit organizations (Cohen and Myers 1950). The 1950 amendments also liberalized the eligibility requirements, making about 700,000 persons immediately eligible for benefits; increased benefits substantially for about 3 million existing beneficiaries, effective September 1, 1950; raised the wage base for tax and benefit computation purposes; and provided a new contribution schedule (SSA n.d. b; Pogge 1952, 9). Without question, these were major changes.

SSA History Museum & Archives.
Unlike its experience with the 1939 amendments, BOASI had a seasoned and well-trained staff to implement the 1950 legislation. BOASI also began preparing for the legislation early and thoroughly. So, although this legislation contained the most extensive changes in the program's 15-year history, BOASI was equal to the task (SSA 1952b).
The Bureau used veteran employees to quickly train new employees, adapted work flows and procedures, and launched an extensive information program to reach potential beneficiaries. As workloads peaked, the Bureau shifted regular employees from one operation to another and used overtime rather than hiring temporary employees (Pogge 1952, 9).
The new coverage provisions meant that millions of new employers and employees had to be registered and wage record accounts established. Forms and procedures for nonprofit organizations had to be developed by January 1, 1951, and interpretations of the law had to be settled to provide states with guidance in framing legislation and negotiating coverage agreements. Forms for reporting self-employment did not have to be finalized until January 1, 1952, but Bureau staff had to work closely with the Bureau of Internal Revenue before then to develop regulations and uniform coverage determinations. An informational booklet with a tear-off coupon for registering household employees was widely distributed, as well as an envelope-style tax return form for reporting household wages. BOASI worked with the Department of Agriculture to distribute information to farm residents (Pogge 1952, 10).
New coverage provisions added new complexity to the program, and additional complexity resulted from legislative provisions to ensure that no one was disadvantaged by changes in program rules. Consequently, already in the 1950s, as many as 16 or 17 different recomputations might be needed. In response, SSA Commissioner Robert Ball initiated a "program simplification" project in the Program Analysis Division. The idea was to have a workgroup examine specific program areas and try to simplify the provisions. The workgroup recommendations to simplify the computations would finally be enacted in the 1960 amendments. This project would be just the first of many SSA attempts to find ways of simplifying Social Security programs (SSA 1996e).
In FY 1951, BOASI awarded benefits to 1.4 million persons, more than twice the previous record. The volume of work had tripled since 1941, and soaring postwar inflation tremendously increased operating costs. Nevertheless, efficiencies the Bureau had implemented enabled it to successfully handle the new workload—although claims processing time increased substantially. The recent introduction of electronic accounting machines supported the mechanical calculation of benefit amounts from punch cards containing wage-record information. By 1951, 47 employees were handling the amount of work that had required 100 persons just 10 years earlier (Pogge 1952, 10).
Because a provision in the 1950 amendments brought about a more liberal benefit computation effective July 1, 1952, many claimants waited until then to file for benefits. As a result, the new claims workload increased by 39 percent. Additional amendments on July 18, 1952, increased benefits for the 4.6 million beneficiaries already on the rolls, and these increases had to be reflected in the September benefit checks. In spite of these additional workloads, the incoming Eisenhower Administration sharply curtailed the Bureau's budgets for the first half of 1953, preventing the Bureau from adding staff to handle the resulting backlogs (OTA 1986, 96).
Implementing the 1954 Amendments
On September 1, 1954, the Social Security Act was amended to extend OASI coverage to self-employed farmers and workers in specified other professions, additional farm and domestic employees, members of state and local government retirement systems on a voluntary group basis, and individual ministers and members of religious orders through election. Additionally, a disability freeze provision4 was enacted to protect the benefit rights of disabled persons (SSA n.d. b).
Area offices worked extensive overtime to compute the benefit increases that resulted from the 1954 amendments. SSA employees had to file an accounting machine-produced form indicating the new benefit amount in each beneficiary's folder. DAO sent employees to each of the six area offices to help. The Philadelphia Area Office, with about 440 employees, worked 2,000 hours of overtime—equivalent to 250 work days—between January 3 and January 11, 1955, alone (SSA 1955b).
To determine farm coverage, SSA had to formulate a policy for measuring "material participation."5 For assistance, SSA turned to the Agricultural Extension Service of the Department of Agriculture and the University of Maryland. SSA policy developers met with county agents and visited farms in the area to speak with actual farm operators about how the program could work. Because Maryland did not represent some farm situations satisfactorily, SSA then expanded its research into Pennsylvania, North Carolina, and Louisiana. Its findings enabled SSA to develop a workable policy (Lowrey 1955, 5). However, covering farmers caused spikes in claims. Once again, the agency temporarily shifted employees to offices where the workloads were the heaviest (SSA 1960a, 34).
In September 1954, the Bureau established the Division of Disability Operations (DDO) to implement the disability freeze. Under a federal-state partnership that exists even today, each state designated an agency to make a determination on disability for applications filed in the local BOASI field offices. The idea behind this state-federal arrangement was to tie the receipt of cash disability benefits more closely to rehabilitation services, which were state functions. Also, Congress did not trust SSA to be strict enough with the medical determinations. SSA paid the state's administrative costs for making the determinations (SSA 1996c). DDO was responsible for negotiations with the state agencies, reviewing state agency decisions on disability, making original decisions for those cases not yet covered by state agreements, establishing standards and procedures for paying the state agencies, and developing medical guides, polices, and training materials for use by both BOASI and state agency personnel. Frequent amendments liberalizing the program posed additional administrative challenges (Christgau 1955, 16).
District offices were also affected, as they had to interview the applicants, complete a medical history, record their observations, and obtain the medical records. In response to the disability freeze, SSA opened a number of new offices, many of them in medium-sized towns and rural areas (SSA 1960a, 34). DDO provided training for the district offices to ensure they were prepared. In January 1955, the Bureau began taking disability freeze applications. There were no special forms for capturing the medical information; employees filled out a long narrative, usually six to nine pages (SSA 1995c). The Bureau had to deal with claims not only from the recently disabled but also from those disabled for many years. The Bureau took half a million claims in just the first few months. The workload in the first quarter of 1955 was equal to the workload for a full year in 1946 (SSA 1955c).
To develop its disability determination policy, DDO staff consulted with the Veterans Administration and the RRB, agencies that already had disability programs (SSA 1996c). Gaining the cooperation and support of the medical community was a major challenge. DDO set up a Medical Advisory Committee, which included prominent private-sector medical doctors suggested by the American Medical Association (AMA), to provide advice and recommendations for disability policy and guidelines. When SSA had the Committee's support, it could usually count on support from the AMA (SSA 1979, 23).
Taking on the Social Security Disability Insurance (DI) Program
On August 1, 1956, the Social Security Act was amended to provide monthly benefits to permanently and totally disabled workers aged 50–64; to pay child's benefits to disabled children aged 18 or older of retired or deceased workers, if their disability began before age 18; and to lower the retirement age to 62 for widows and female parents. In November 1956, retirement benefits also became payable to women at age 62 (SSA n.d. b).
The passage of DI benefits was extremely controversial, with many special interest groups vociferously opposed. Congress and the Eisenhower Administration expressed concerns about potential program costs and encouraged SSA to take a "strict" approach to administering the new benefits. However, constituent complaints about the high disallowance rate prompted Congress to hold high-profile hearings on the disability program in 1958. As a result, some administrative procedures and policies were made less restrictive. In addition, following these hearings, SSA published its disability medical listings6 for the first time (SSA 2001b).

SSA History Museum & Archives.
Use of state agencies to make the disability determination was continued in the 1956 legislation. However, although the state agencies decided whether a person's impairment met the requirements for disability benefit entitlement, DDO reviewed every decision (SSA 1995e).
With increased workloads in the district offices came heavy claims loads in the payment centers. The number of beneficiaries grew from 9.1 million in 1956 to almost 12.5 million in 1958. Although Bureau employment grew from 18,000 in 1956 to 22,500 in 1958, ingenuity and new, more efficient processes were required to cope with the additional work (SSA 1960a, 34).
Trying New Technology
In the 1950s, the United States entered the computer age, and SSA once more was a leader in adopting new technology. In 1950, the Bureau installed its first "high-speed electronic calculator" for claims processing (FSA 1950, 32). In July 1955, the Bureau acquired an IBM 705 II Data Processing System for posting earnings, computing benefits, and reinstating incorrectly reported earnings items (SSA 1960c; SSA 1964b; SSA n.d. b). On July 1, 1956, the earnings posting operation changed from an 80-column IBM punched card and the IBM 407 Accounting Machine to electronic data processing equipment which stored information on magnetic tape using a binary code. One reel of magnetic tape could hold the information from almost 32,400 punched cards, and the Summary Card File alone had 120 million records to be converted to tape (SSA 1960c, 20–21).
SSA also helped pioneer a microfilm printer that linked computer and microfilm technology (OTA 1986, 99). Until 1958, the Bureau was still using the Flexoline to keep track of SSNs issued. The mammoth file took up a city block of floor space. It was growing at the rate of about 3 million names a year and required 6,000 additional square feet of space every 12 months. SSA plainly could not continue using the Flexoline file indefinitely. In 1958, the existing National Employee Index was microfilmed. By 1964, the 200 million names in the National Employee Index were contained on 2,005 reels of magnetic tape divided among about 90 "stations," each equipped with high-speed microfilm readers (SSA 1964b).
1960s
After responding to the challenges posed by extensive growth in the Social Security program in the 1950s, SSA was poised for additional challenges in the 1960s. The biggest of these was tackling an entirely new program—Medicare.
SSA also underwent a major organizational change. On January 28, 1963, SSA shed many of its former responsibilities when HEW moved the Children's Bureau and the Bureau of Public Assistance into a new Welfare Administration. SSA's role would now be essentially identical with that of the now-abolished BOASI, focusing primarily on the retirement, survivors, and disability insurance programs.
In March 1965, further organizational changes at SSA created four program bureaus: The Bureau of Retirement and Survivors Insurance, the Bureau of Disability Insurance (BDI), the Bureau of Health Insurance, and the Bureau of Federal Credit Unions. SSA also created a Bureau of Data Processing and Accounting—later shortened to the Bureau of Data Processing (BDP)—that assumed responsibility for the operational functions of the former DAO (SSA n.d. b).
Maintaining Public Service
In 1961, the agency's workforce provided 25,829 "man-years" of service, of which 11,473 were dedicated to processing claims and about 5,000 were spent posting wages. BOASI had 11 regional offices, 584 district offices, and 3,541 contact stations (previously called itinerant stations). Field offices still took claims, developed the evidence, and sent the applications into the seven payment centers for final adjudication and certification of payment to the Treasury Department. More than 35 days typically elapsed between taking an application for benefits and payment certification. Of this time, 6 hours was for BOASI employees' direct work and the rest was spent physically moving materials from one work station to another or awaiting evidentiary documents (Ladd and others 1961; Futterman 1960, 2).
SSA was considered a well-run organization. A report of the 1965 Advisory Council on Social Security stated:
From our own observations and from the evaluation of others, we believe that the huge task of administering the social security program, a task which involves the rights of many millions of people and the payment of billions of dollars a year, is being handled effectively and efficiently.
Administrative costs have been kept down to only 2.2 percent of benefit payments, partly as a consequence of the use of the latest in methods and machinery. This low administrative cost, however, has not been achieved by sacrificing high-quality service to the public. Employees at all levels have combined efficient performance of duties with responsiveness to the public and a friendly and sympathetic concern for the aged, the disabled, and the widows and orphans who are the program's beneficiaries.
We would like to register our belief that accomplishment of the purpose of the social security program requires that this high quality of administration—nonpartisan and professional—be continued (Advisory Council 1965, 39–40).
SSA employees' dedication to serving the public would be a factor in successfully handling its next big challenge: implementing the 1965 amendments. As an initial step, the Commissioner in 1965 approved the establishment of branch offices under the direction of the District Office Managers (SSA n.d. b).
Launching Medicare
The 1965 Amendments to the Social Security Act, enacted July 30, provided hospital insurance (HI) to persons aged 65 or older who were entitled to monthly Social Security retirement benefits, as well as to unentitled individuals who would reach age 65 before 1968 (Medicare Part A). All persons aged 65 or older were also permitted to voluntarily purchase Supplemental Medical Insurance (SMI) for physician's services (Medicare Part B). Medicare was to go into effect July 1, 1966, giving the agency less than a year to implement the program.
Simultaneously, the agency had to implement changes to the OASDI program. The new law extended eligibility to students, divorced wives, and widows aged 60 and liberalized the retirement test and the definition of disability. It also instituted a "transitional insured status" for persons who reached age 72 before 1969. In addition, it provided a 7-percent increase in benefits retroactive to January 1, 1965.
Coverage in the voluntary SMI program was to begin July 1, 1966. The enrollment deadline for those aged 65 or older was March 31, 1966. Late enrollment would result in delayed coverage and a premium penalty. Persons attaining age 65 after March 31, 1966, had to enroll during the 3-month period preceding their 65th birthday. The SMI premium of $3 a month was to be deducted from the Social Security benefit check.
The effort required to create the Medicare program while simultaneously implementing the OASDI benefit portion of the 1965 legislation was staggering. First, 19 million potential Medicare beneficiaries had to be identified and contacted to determine their eligibility. SSA staff had to elicit and process SMI enrollment forms. The agency also had to prepare and certify those who would be providing hospital and medical services covered under HI and SMI. SSA had to develop contracts with the intermediaries that would handle reimbursement for hospital services rendered and also with the carriers that would determine "reasonable charges" and handle the reimbursement for SMI services. SSA needed an administrative infrastructure for Medicare, which required hiring and training 9,000 employees, setting up 100 new field offices, coordinating activities with numerous other federal agencies, and developing internal systems capacity. In addition, SSA had to develop Medicare program policy through consultation with other agencies and many interest groups (Ball 1965; Gluck and Reno 2001, iv–v).
Commissioner Robert Ball later attributed the Agency's success in implementing Medicare to three factors: an existing nationwide organization that was disciplined and experienced in dealing with the public, had high morale, and was eager to do the job; a group of central planners and leaders with enthusiasm, imagination, and quality leadership skills; and an almost complete delegation of authority and responsibility to SSA from higher levels (Gluck and Reno 2001, 9–10).
Shortly after the legislation was signed, SSA mailed a punch-card application form together with an information pamphlet to all Social Security, civil service annuity, and railroad retirement beneficiaries who were within 3 months of their 65th birthday or older. SSA also obtained leads from the Internal Revenue Service (IRS, successor to the Bureau of Internal Revenue), welfare rolls, state and local retirement plan agencies, nursing homes—any source that could provide a list of names and addresses for the elderly. Two follow-up mailings went out to nonrespondents. SSA also hired advocacy groups for seniors to go door-to-door. Even the Forest Service was enlisted to look for people camping out in the woods (SSA 2001b; SSA 1995b).
SSA distributed over 120 million booklets about Medicare and sent a continuous flow of materials to the media, which provided unstinting support throughout the initial enrollment period. Newspapers printed column after column on the new program; radio and television stations presented live and recorded programs explaining the law; and post offices widely displayed posters. The number of news items ran into many hundreds of thousands. District office employees made nearly 90,000 talks, 194,000 radio broadcasts, and 5,000 live television appearances; they also manned 29,500 exhibits (HEW 1966, 21).
To accommodate those wishing to enroll in Medicare, SSA opened 9 additional district offices, 74 branch offices, 12 resident stations, and 21 temporary service centers. By the end of 1965, there were 725 district offices, 82 branch offices, 37 resident stations, 16 service centers, and 3,361 contact stations to serve the public. The new branch offices were located not only in rural areas that were remote from existing district offices, but also in metropolitan areas with large populations of minorities and disadvantaged individuals. In addition, many existing offices were enlarged to accommodate new staff (SSA n.d. a). Still, the offices were overflowing with staff and claimants. Some offices conducted mass interviews, taking 20 to 30 enrollees into the training room, giving each an application, and walking through the questions while enrollees completed the forms (SSA 1995d).
As the March 1966 deadline approached, SSA's field offices extended their hours for those who still wanted to apply. Some offices stayed open until midnight in the last week or two while others were open on weekends (SSA 1996a). President Lyndon Johnson signed a proclamation designating March 1966 as "National Medicare Enrollment Month." On April 8, 1966, legislation extended to May 31 the deadline for filing SMI applications, with coverage to take effect July 1, 1966 (SSA n.d. b).
At the same time it was enrolling beneficiaries, SSA had to contact every hospital to certify that it met Medicare requirements and complied with Title VI of the Civil Rights Act. One result of this effort was the nearly complete desegregation of U.S. hospitals. The agency also had to provide information to every doctor in the country, explaining the program and encouraging them to participate (SSA 2001b).

SSA History Museum & Archives.
Planning the operational flow for admitting Medicare patients to hospitals required extensive discussions with insurance companies, hospitals, and other experienced organizations. Procedures for processing physician's bills were needed. Contracts had to be developed with the organizations that would process and review the bills and send out explanation-of-benefits notices (SSA 1995b).
The effort was not without problems, but SSA succeeded, and Medicare went into effect as scheduled on July 1, 1966. By that date, SSA had enrolled about 19.1 million HI beneficiaries and 17.3 million SMI enrollees (HEW 1966, 10). The agency had enlisted 6,800 hospitals, 4,000 extended care facilities, over 1,800 home health agencies, 2,400 independent laboratories, and 750,000 private physicians as Medicare participants (SSA 1967b, 4–5).
SSA continued to administer Medicare until 1977, when SSA's Bureau of Health Insurance split off to become a new agency, the Health Care Financing Administration—which has since been renamed the Centers for Medicare and Medicaid Services (CMS). The nature of the Medicare-related administrative problems that the Bureau faced until 1977 are beyond the scope of this article, but the sheer size of the Medicare workload affected SSA's ability to administer OASDI.
SSA processed and distributed the retroactive and ongoing OASDI benefit increases mandated by the 1965 legislation accurately and on time, but the new OASDI provisions presented another major workload. The 1965 amendments provided for automatic recalculation of benefits for OASI beneficiaries who had continued to work after entitlement. Extensive planning and preparation were required to identify eligible individuals and to recalculate their benefits; most recalculations were automated but many were done manually (SSA n.d. a). The seven payment centers were overwhelmed during this period. OASDI awards increased nearly 1.5 million to 4.1 million, not counting 1.1 million lump-sum death payments in FY 1966 (HEW 1966, 17). The following year, the number of initial claims filed more than doubled, to 8.5 million. These new workloads were superimposed on substantial increases in the volume of work already seen in payment centers over the preceding few years (SSA n.d. a). The payment center work regimen had become antiquated and unwieldy, and was not equal to the new demands (Bowers and Korycki 1970, 28–29; SSA 1996a).
Other agency workloads also increased. In FY 1966, SSA posted 282.5 million earnings items (an increase of 5 million from FY 1965), issued 6.8 million new SSNs (up 1.8 million), and issued 3.5 million replacement Social Security cards (HEW 1966, 17). All the while, Congress was preparing further legislation for 1967.
Coping with More Legislative Changes
The impact of the 1967 amendments on SSA operations would not be nearly as large as that of the 1965 amendments, but considering the strain on resources brought about by the earlier legislation, the agency once again planned its response in advance.
In the fall of 1966, Commissioner Ball requested all operational elements to evaluate their readiness and to have regular program workloads in the best possible shape by the middle of January 1967. The agency took several courses of action. Overtime hours had been used in implementing the 1965 amendments, and would be used again now. Payment center employees worked nearly a million hours of overtime during FY 1967. Field offices pitched in to help the payment centers. District office claims representatives were detailed to the payment centers in New York, Chicago, and Philadelphia, where the greatest problems existed. Also, field office personnel worked overtime on Saturdays and Sundays in payment centers. Central office teams were sent to three payment centers in September 1966 to observe operations and returned with suggested improvements (SSA n.d. a).
Workload challenges increased with staff reductions mandated by the Revenue and Expenditure Control Act of 1968, which cut nearly 2,000 full-time positions from SSA's workforce in 2 years, from 52,459 to 50,488, while workloads increased 10 percent. Additionally, President Richard Nixon ordered that total federal employment be reduced by 5 percent and that all agencies reduce the average grade level for employees. The staffing cuts had a noticeable effect on SSA operations. Imbalances developed, especially in clerical jobs, resulting in uneven quality of services provided (OTA 1986, 96; SSA 1969, 16; House Ways and Means Committee 1973, 3).
The decade closed with 1969 amendments requiring a benefit conversion for 24.8 million OASI beneficiaries effective January 1970. Although SSA was able to automate about 97.5 percent of conversions, over 600,000 records still required manual computations. Once again, SSA diverted resources. Benefit increases were sent out by April 1970, as required, but the cost was that other pending workloads rose (SSA 1969, 16–17; SSA 1970, 59).
1970s
By 1970, SSA had a stellar reputation as an agency that could handle anything demanded of it. However, SSA would stumble in the 1970s as it attempted to implement SSI. With only 14 months to put a whole new program and its computer system in place—just after having implemented Black Lung benefits, another entirely new program—SSA's task was simply too large to carry out without setbacks.
Changing the Claims Process
Although SSA's productivity improved 16.1 percent between 1967 and 1972, the agency was strained. SSA began to experience its first mass staff losses in the late 1960s, as employees who had started with the agency in the 1930s and 1940s started to retire (House Ways and Means Committee, 1973, 3).
To mitigate the impact of staff losses and to improve efficiency, SSA took steps such as expanding the use of telephone interviews. By the end of 1971, 30 percent of claims and postentitlement changes were handled by phone (SSA 1971, 8). SSA also started using private organizations such as employers and unions in the preclaims and claims process, enlisting over 3,000 employers. Use of microfiche for beneficiary records was expanded; by mid-FY 1970, all 800 field offices had microfiche readers. SSA also initiated "simultaneous development" of disability claims in field offices and state agencies (SSA 1970). Until 1971, field offices collected all medical evidence before sending a claim to the state agency for a disability determination. Starting in late 1970 and expanding over the next couple of years, field offices collected only the names and addresses of medical sources, and the state agencies obtained evidence. This one change reduced average DI processing days from 93 to 66 and required fewer consultative medical exams (House Ways and Means Committee 1973, 8; SSA 1995e).
The real problems were in the payment centers. In 1973, the centers handled a 20 percent increase in all OASDI benefits, including 4.3 million increases in widow's benefits. Staff overtime increased 56 percent, to 883,000 hours (SSA 1973b, 61). To alleviate payment center backlogs, SSA reduced the number of claims requiring authorizer review. Since 1937, every claim received in field offices had been mailed to another location for payment authorization. Experience had shown that the processes of gathering evidence and making the entitlement decision were so closely related that in most cases, field employees were making the same judgments and decisions as adjudicators. By providing field employees with the earnings record and having them complete the determination form previously executed by the adjudicator, SSA eliminated some handling in the Claims Division. Starting in September 1941, a claims representative in a district office not only took the claim, but also completed an SSA-101 award determination form reflecting the findings of fact and decision, although this did not authorize payment. The claim was then forwarded to a claims authorizer or examiner in the area office (payment center) to make the formal entitlement determination. State agencies made the disability determination (SSA 1966).
In March 1969, SSA authorized field office employees to make payment decisions for certain initial claims under the District Office Final Authorization (DOFA) procedure. Field offices were first authorized to adjudicate selected lump-sum death payment cases. In April 1969, this delegation was expanded to authorize field offices to adjudicate certain OASI claims with computer-generated awards (House Ways and Means Committee 1973, 7). By FY 1970, field office employees were authorizing 43 percent of initial claims (SSA 1970, 19). In May 1972, SSA began selecting cases for DOFA based on "conspicuous characteristics;" DOFA was used in 67 percent of cases by June 1972, and in 74 percent of cases by 1974 (House Ways and Means Committee 1973, 8; SSA 1974b, 16).
However, even when field office claims representatives were authorized to trigger payments, technological limitations still required manual handling in the payment centers—which by 1976 had been renamed program service centers (PSCs). In 1977, 25 percent of claims required some manual processing. For these cases, field offices still filled out a paper form SSA-101 and sent it to the PSC for keying into the system (Casey 1977, 13). In 1979, 1.8 million of SSA's 3.7 million Retirement and Survivors Insurance claims still required manual PSC handling to initiate payment.
While the PSCs struggled, BDI was drowning. The PSCs took over additional work from the overwhelmed BDI, assuming jurisdiction for disability claims and records for beneficiaries aged 62 or older. Transferring the folders from BDI to the PSCs began in 1977 and was completed by April 1978. This transfer reduced by over 600,000 the number of records under BDI's jurisdiction and freed BDI resources to deal with increasingly heavy disability workloads (SSA 1975c, 48).
The 1977 amendments, although not taking effect until 1979, nevertheless brought immediate additional OASI workloads. They created delayed retirement credits (DRCs) for actuarially reduced beneficiaries who continued to work after age 65, increased remarried widow benefits from 50 to 100 percent of the primary insurance amount (PIA), and instituted a special minimum PIA increase from $9 to $11.50 per coverage year. These provisions would increase payments to 1.2 million beneficiaries in 1979 (SSA 1980a).
Administering Black Lung Benefits
On December 30, 1969, President Nixon signed the Federal Coal Mine Health and Safety Act, putting the Black Lung (BL) benefits program into place, effective immediately. This legislation authorized monthly cash benefits to coal miners who became totally disabled because of pneumoconiosis (black lung disease), as well as to their dependents and survivors. Congress made SSA responsible for the payment and administration of BL benefit claims filed under Part B rules through December 31, 1973 (with certain exceptions), with the Department of Labor (DOL) to take responsibility for claims filed under Part C thereafter (SSA n.d. b).
SSA was not advised of the legislation until December 9, 1969 (SSA 1995c). BDI staff had to develop a substantial body of policies and procedures to implement the nonmedical provisions of the law and to ensure those provisions were reflected in published regulations. Publication of the regulations was not complete until March 4, 1971 (SSA 1971, 79).
With no retroactivity for benefits payable, coal miners did not wait for regulations and procedures. They began trooping into district offices January 2, 1970. Thirty small field offices in coal mining regions bore the brunt of the workload; five would receive more BL claims during the first 2 weeks of the program than their normal annual receipts for all types of claims. Miners filed some 80,000 claims in January 1970 alone, and 172,000 by July 1, 1970. BL applicants from Appalachia frequently filed for OASDI benefits as well. Once again, SSA kept field offices open evenings and weekends to accommodate the applicants. SSA also brought employees in from other field offices and from the Disability Determination Services (DDSs, formerly known as state agencies) to assist (SSA 1970; SSA 1995c).
For BL claims, as with DI claims, DDSs requested the available medical records. However, the primary resources needed to process the claims were in BDI where the BL claims went for final processing. The decision-making process was very labor intensive. X-rays required two or three readings by examiners who had received special radiology training. Many decisions involved a disability onset or death that had occurred years before. Pressured by a few Congressmen representing coal mining districts, SSA put more and more resources into BL claims, creating a backlog of disability claims. SSA suspended Continuing Disability Reviews (CDRs)7 for 2 to 3 years to devote resources to the BL claims, a decision that would have serious consequences later (SSA 1995g; SSA 1979, 25).
By May 1972, SSA had taken 366,000 BL claims and made 350,500 decisions, of which only 159,500 were awards. To permit more awards, Congress significantly broadened the eligibility provisions of the 1969 law in the Black Lung Benefits Act of 1972, enacted May 19 (House Ways and Means Committee 1973, 21). Stimulated by the program amendments, miners filing BL claims numbered 192,200 in FY 1973 and 149,000 in FY 1974 (SSA 1973b, 20; House Ways and Means Committee 1974, 25). SSA was also required to reexamine and, in many cases, redevelop all the previously denied claims. In addition, SSA had to handle appeals for denied claims—8,000 reconsiderations and 3,800 hearings in FY 1973 (SSA 1973b, 23).
In July 1973, responsibility for processing new BL claims (Part C of the BL program) transferred to DOL. However, SSA retained responsibility for the BL beneficiaries who filed before then—a caseload numbering 338,385 miners, their dependents, and survivors as late as September 1983 (House Ways and Means Committee 1974, 3; SSA 1984a, 4). On January 1, 1974, SSA began taking BL claims for DOL on a reimbursable basis (SSA 1974b, 1). By June 1974, SSA was still taking about 4,000 BL claims per week, up from 2,000 before the 1972 amendments (House Ways and Means Committee 1976, 26). SSA took 523,000 BL claims for DOL in FY 1973 and 556,000 in FY 1974 (SSA 1974b, 24). The BL workload did not decline significantly until 1975 (SSA 1975c, 23).
The Federal Mine Safety and Health Act of 1977 further liberalized the program by requiring SSA to review again all the claims it had fully or partially denied. This created another huge workload as SSA had to track down hundreds of thousands of individuals whose claims had been denied according to provisions of earlier amendments.
Implementing SSI
SSA implemented Medicare so successfully that, a few years later, the agency seemed a logical choice to administer a federal program providing aid for the aged, blind, and disabled with limited income and resources. Such programs had previously been administered by the states with some federal funding.
President Nixon signed the Social Security Amendments of 1972 creating the SSI program on October 30, 1972, only 14 months ahead of the January 1, 1974, effective date. SSA estimated that 3 million people would be converted from the 50 state welfare rolls to SSI. In addition, SSA expected to take in another 3.3 million new applications because the SSI eligibility standards were more generous than many state programs (House Ways and Means Committee 1973, 41). The law also made changes in the OASDI and Medicare programs.
SSA was selected to federalize welfare for adults for a number of reasons: its nationwide network of field offices was already in place, its data processing and recordkeeping system was considered state-of-the-art, and there was overlap between the OASDI and SSI populations. Because of this overlap, it was thought the new program would not unduly burden SSA (SSA 1994a, 5). In fact the programs were fundamentally different. OASDI benefits were based on a worker's earnings history, while SSI payments were based on income and resource limits. In addition, OASDI applicants generally filed a few weeks to 3 months before entitlement, while eligible SSI applicants were entitled to immediate payments upon filing (SSA 1995h).
For SSI, the agency not only had to set up a new program from scratch, as with Medicare, it also had to bring 50 state programs—each of which had different eligibility criteria, standards, and payment levels—into a single system. All of the state records were flawed in some way, and some state recordkeeping systems were extremely lax. Some states still had only paper records. The task of converting the state recipients to SSI was aggravated by the legislation not giving SSA adequate clout for dealing with the states, some of which were openly antagonistic. In addition, SSA was made responsible for administering state programs to supplement SSI for those states that so opted. In effect, SSA had dozens of new needs-based programs to administer rather than just one (SSA 1996b).
SSA set up a new Bureau to develop SSI policy. BDP was tasked with building a new computer system, and the Bureau of District Office Operations was to implement the program. Ten regional planning officers were appointed to work directly with state and county welfare agencies. By June 1973, SSA had established regional cadres, 200 people in all, to negotiate with states. In addition, SSA set up a central office Systems Planning and Development Work Group with representatives from all SSA components to discuss SSI activities and to initiate systems development (SSA 1973b, 5; House Ways and Means Committee 1974, 38; SSA 1996b; SSA 1994a).
Developing SSI policy was more complex than SSA had anticipated, especially in the areas of in-kind support and maintenance, living arrangements, attribution of income of spouses and parents living in the household ("deeming"), eligibility of drug addicts and alcoholics, and state supplementation variations (House Ways and Means Committee 1975, 14). SSA's work was further complicated by legislative changes made after enactment of the 1972 amendments. These changes included blanketing in additional groups of individuals, such as "essential persons;"8 mandatory state supplementation of certain recipients converted from the state programs; increases in benefit amounts effective January and July 1974, enacted on December 31, 1973; and a requirement to review the disability of all persons added to the state disability assistance rolls during July–December 1973 (House Ways and Means Committee 1975, 13).
SSA's initial estimate of needing 18,000 additional employees to administer SSI was scaled back to 15,000 by the Nixon Administration. SSA was ultimately authorized to hire an additional 12,000 permanent staff in 1973: 9,000 for SSI and 3,000 for the other programs that SSA administered. SSA opened 159 branch offices and expanded several hundred existing offices in FY 1973 and was authorized to open another 180 branch offices in 1974 (104 to meet SSI needs and 76 for existing needs), bringing the number of field offices to 1,085. SSA also opened seven new teleservice centers (TSCs) in FY 1973 and eight regular TSCs and seven "mini-TSCs" in FY 1974 (SSA 1973b; SSA 1974b, 4; Derthick 1990, 119; SSA 1994b).
Congress' original intent was for SSI to establish a national system with uniform payments and rules, but it soon became evident that this would disadvantage many current recipients in states with higher costs of living and higher welfare payments. In the original legislation, Congress encouraged states to supplement the federal law, but doing so was not mandatory. The 1972 legislation failed to hold individual recipients harmless—that is, nothing required that the state's prior level of payment be maintained.
In the summer of 1973 Congress finally realized that recipients in about half the states would receive less under the federal SSI program than they had under state programs. For instance, some states provided higher welfare payments to account for family members in the recipient's household who were themselves ineligible but were considered essential to the recipient. In July, Congress amended the 1972 law via Public Law (P.L.) 93-66 to cover these "essential persons," which had the effect of increasing the recipient's SSI payment by adding a monetary supplement for each essential person the state had designated. Congress also threatened to withhold Medicaid grants to states unless they protected individuals against harm (Derthick 1990, 74).
SSA was very busy negotiating with the states during 1973. In some states, individual counties (or other jurisdictions) ran their own programs, and SSA had to negotiate separately with each jurisdiction. Rather than creating a uniform set of rules for the state supplementation programs it agreed to administer, SSA accepted numerous variations, such as allowing differences among categories of recipients, up to three zones within a state, and five different living arrangements. SSA agreed to these state variations in hopes that states would choose federal administration of their supplements, and would choose quickly. However, SSA lacked the bargaining power to induce the states to do so on its terms, and so accepted the state terms. As the number of variations increased, so did the complexity of the computer software, the amount of processing time required, the training needs, and the costs; SSA's administrative control simultaneously decreased. Some states gambled that by delaying decisions to the critical point they could pressure SSA into accepting variations that SSA resisted, and their gamble paid off. It was not until December 18, 1973—only 2 weeks before implementation—that the last of the states made its final decision (Derthick 1990).
Meanwhile, regular staff and some temporary hires at 1,350 state, county, and local welfare offices were filling out the computer input forms used to convert their beneficiaries to SSI (House Ways and Means Committee 1975, 13). Full-scale conversion began in February 1973, and by June 1973 SSA had received 2.8 million computer input records. SSA received an additional 1 million records by December 31, 1973, including about 700,000 new beneficiaries that states added to the rolls in the second half of 1973. There were major problems: The information in many state and county files was out of date, and transcription errors also generated bad data (SSA 1975c, 36; SSA 1984b).
To comply with P.L. 93-66, SSA developed new procedures to gather the required data on essential persons and ineligible spouses. The states submitted information on over 177,000 essential persons and 154,000 ineligible spouses, parents, and children, which SSA screened and added to its records. In November 1973, SSA sent all the records from its Conversion Master Files to the states to be rechecked against the state files to ensure that SSA had records of all state recipients. The states responded with any additions and deletions (SSA 1975c, 37).
Many of the state welfare beneficiaries and essential persons had never been issued an SSN. SSA initially estimated that 800,000 state beneficiaries would need a new SSN, requiring 935 man-years of keypunching operations and 555 clerical man-years to process them—a 70 percent increase in such workloads. SSA set up a keying center in Albuquerque to handle these new demands (SSA 1973b).
BDP checked the SSN in every state conversion case record it received and in the new SSI claims inputs. The Bureau found 745,000 cases in which the state-supplied SSN data could not be verified. SSA mailed a questionnaire to each of these individuals. The responses provided SSA with correct SSNs or allowed SSA to issue an SSN in 501,000 instances. The states also mailed in new SSN applications (SSA 1975c, 37). In spite of these efforts, when the SSI program began, thousands of SSI records lacked a genuine SSN and had to be controlled under temporary "pseudo-numbers" (9-digit numbers beginning with a "9").
During 1973, SSA also undertook a public relations effort to inform the public about the program. SSA's Office of Public Affairs briefed representatives of 128 national organizations and agencies on SSI and issued 45 informational publications. Field offices held 37 exhibits at national conventions and created many new radio and TV spots in the first half of 1973. SSA field offices began taking new applications for SSI on July 2, 1973 (SSA 1973b, 80), and had taken 2.9 million new applications by the end of the year (House Ways and Means Committee 1976, 35).
Still, there were fewer new applicants for SSI than SSA had anticipated. To reach potential applicants, SSA began phase I of "SSI Outreach" in November 1973, with the U.S. Agency on Aging providing $6 million for advocacy groups to get the word out (House Ways and Means Committee 1975, 9). At one point, SSA had 55,000 volunteers distributing literature and explaining the basic eligibility requirements of SSI. Based on the leads collected by volunteers, SSA had by the end of 1973 contacted 107,000 individuals, of whom 42,000 filed claims for benefits. An additional 250,000 leads had been screened out as ineligible, and about 50,000 leads remained to be contacted.
SSA then began SSI Outreach phase II, sending an information leaflet and questionnaire to 5.2 million OASDI beneficiaries with payment amounts low enough to be within the SSI income limit (SSA 1974b, 5). SSA also put SSI announcements in more than 1,300 newspapers and aired more than 4,000 radio spots. By June 30, 1976, 1.5 million newly eligible persons comprised almost 37 percent of SSI recipients (House Ways and Means Committee 1976, 34).
SSA planned to set the new SSI computer system up in 10 stages (SSA 1973b, 6). Because of the complexity of the SSI program and the many variations of federally administered state supplements, 100 separate software systems with nearly 1 million individual instructions were required, making the new system one of the largest and most complex computer operations in the country at that time (Derthick 1990, 86). Among the requirements were an automated system to process information, maintain recipients' records, and calculate monthly benefits; a telecommunications system enabling the 1,400 field offices to send data to centralized computers; and a system for transmitting information needed by states to make state-administered supplemental payments and to determine Medicaid eligibility (Derthick 1990, 29).
From the start, SSA set up the SSI program to enable field offices to adjudicate claims and key in the data that would trigger payment, bypassing PSC authorization and processing. Field office employees converted the information from the paper applications onto a data entry form used by the office teletypist to enter into the SSI system. The system maintained these entries in a "pending" file where they awaited the creation of the payment certification file to be sent to the Treasury Department in December 1973, which enabled timely postal delivery of the January 1974 payments on January 2.
However, programming the new software was hampered by the four 1973 legislative changes and by some states exercising the option of federal administration of state supplements at the eleventh hour. As a result, SSA was still creating code until the last minute and did not have sufficient time to test the new software programs before they went operational (SSA 1975c, 33). When SSI went into effect, some of the systems for executing and updating claims and payments were not functional. On January 2, 1974, SSA issued timely and correct SSI payments to 95 percent of the SSI recipients, but 5 percent did not get paid or were paid an incorrect amount. As late as June 30, 1974, at least 38,418 conversion cases would still remain to be processed (SSA 1975c, 36). To exacerbate problems, the software for recording certain changes (including changes to income or resources that affected payment) was not in place. Changes for conversion cases submitted by states and counties had not been processed. Furthermore, if a critical error caused the rejection of either a conversion record or a new claim input record, there was no way for field employees to correct the bad record. SSA's computer systems and high-speed communications equipment had failed to perform as well as needed (House Ways and Means Committee 1976, 35).
As a result, when SSI began in January 1974, chaos erupted, particularly in some of the large metropolitan offices—notably New York City, Seattle, and San Francisco. Thousands of people poured into the offices at once. An office would often have all the people it could handle for the day within 15 minutes of opening. Those arriving later were given a ticket or chit signifying priority status for the following day (SSA 1974b, 4; SSA 1975c, 35–36; Hensley 1994).
New York City was especially hard hit. It was winter, and the temperatures were freezing. SSI recipients with payment problems spilled out of the offices into the biting cold. On January 9, 1974, SSA chartered 22 heated, restroom-equipped buses to provide shelter for the people waiting outside New York City offices. In March, SSA set up 4 temporary New York City interviewing facilities, furnishing them with the needed supplies, equipment, furniture, and 250 employees within 2½ weeks (SSA 1974b, 4; SSA 1975c, 35–36; Hensley 1994).
SSA also set up a procedure for issuing one-time emergency payments. In addition, district offices used "imprest funds" via prepositioned checks to make advance payments up to $100 to those converted from state rolls who did not get their payments (SSA 1975c, 35). About 600 SSA employees from other field offices, regional offices, the PSCs, and headquarters were temporarily reassigned to field offices with the heaviest SSI workloads. Some PSCs took on part of the OASI workloads from selected field offices. In addition, SSA budgeted for about 233,000 hours of overtime per week during 1974 (SSA 1975c, 35; SSA 1995h; SSA 1994b; Hensley 1994).
The new SSI software was not the only computer system failure. SSA had also created its first online database, providing field employees with access to information on SSI recipients. SSA designed this database assuming a peak load of 20,000 transactions a day. System demand exceeded 60,000 during its first week and would soon reach 80,000. Field office employees queried the SSI database 106,348 times the first week of January, and by February 19, queries had climbed to 1.26 million. As a result of the unexpected volume, the whole system went down for extended periods, and the telecommunications system collapsed. The Bureau of District Office Operations set up an emergency control center with 26 teletypists to take field office requests for payment status information when the telecommunications system was down. At first, the control center employees phoned the information to field offices, but as the volume of emergency requests rose, they teletyped their replies (SSA 1995h; SSA 1984b; SSA 1994b).
SSI conversion "rollback" cases presented yet another workload. In late 1973, Congress became concerned by the hundreds of thousands of new adult welfare recipients that states and counties were adding to the rolls of those converting to SSI. One result was a provision in December 1973's P.L. 93-233 to "roll back" cases added to the rolls after June 30, 1973, requiring SSA to make new disability determinations. All "rollback" disability decisions were to be made by March 31, 1974, a deadline SSA failed to meet. By June 30, 1974, SSA had identified 144,000 rollback cases and completed 126,700 determinations, in which 90,000 were found eligible (House Ways and Means Committee 1975, 26–27).
Implementing the drug addiction and alcoholism (DA&A) provisions of SSI legislation also created more work for the agency. Sanctions precluded drug addicts and alcoholics from receiving payment in any month they refused treatment; they were also required to receive payments through a representative payee. In November, the Secretary of HEW approved an SSA recommendation that the sanctions only apply to those entitled to SSI disability benefits substantially on the basis of addiction or alcoholism. SSA undertook to review all cases in which DA&A was a factor (except in New York City, where a sample review of the coding showed records were essentially correct). At midyear, SSA directed DDSs to give top priority to this screening and to the preparation of medical determinations for the rollback cases involving DA&A. By the end of FY 1974, the DDSs had processed more than 20,000 of the estimated 27,000 DA&A-involved rollback cases. In addition, SSA worked through HEW with the state vocational rehabilitation agencies to set up treatment and monitoring programs to comply with the DA&A requirements (SSA 1975c, 38).
SSA continued to add new recipients to the SSI rolls even as it sought to straighten out the payments for those already entitled. By June 30, 1974, SSA had taken 1.8 million SSI initial claims, but of these, 293,538 were duplicates or otherwise not countable. More than 953,000 of the initial claims were for disability benefits (House Ways and Means Committee 1975, 25). Only 666,270 of the initial claims had been allowed by June 30, with another 480,420 pending a decision. Conversion cases totaled 3.4 million, of which 38,418 were still not processed as of June 30, 1974. As of that date, there were 3.6 million SSI recipients in current-pay status; by year-end, this number had increased to 4.0 million, and the pending SSI cases had dropped to 335,363 (House Ways and Means Committee 1975, 11).
By FY 1975, there were 4.1 million SSI recipients, up 16.3 percent from FY 1974. In 1975, SSI old-age claims declined 29.4 percent from 1974, but SSI blind and disabled claims were up 24.3 percent, to 1.2 million (House Ways and Means Committee 1976, 32). To speed payment to needy blind and disabled claimants, SSA implemented a "presumptive disability" decision process for certain impairments, such as blindness, which allowed payments for up to 12 months pending the DDS decision; if the recipient was found not disabled, repayment was not required (House Ways and Means Committee 1975, 26).
Once the initial problems were under control, SSA had to begin SSI eligibility "redeterminations" of all recipients, starting with the state conversion cases. SSA had underestimated the complexity of maintaining the beneficiary rolls for a program based on income and resources. One indication was that this work was initially assigned to GS-6 service representatives rather than GS-10 claims representatives (SSA 1973b, 51). Soon, both claims representatives and service representatives were conducting redetermination interviews to deal with the volume of work involved. Because there was not enough time to conduct the redeterminations during the regular workweek, it was not uncommon to schedule interviews all day Saturday (SSA 1984b). By June 30, 1975, SSA field offices had processed more than 2.1 million conversion redeterminations, with 82.3 percent resulting in no change in eligibility or payment status; about 483,000 cases remained to be reviewed (House Ways and Means Committee 1976, 34).
By FY 1976, SSA had most of the needed postentitlement automated procedures in place and had completed over 15 major enhancements to the basic SSI claims payment system (House Ways and Means Committee 1976, 35). Things were just beginning to normalize.
Coping with the Extended Impact of Implementing SSI
Just as implementing BL benefits created increases in other workloads and strained agency resources, implementing SSI produced collateral impacts. For the first time since 1963, SSA's productivity decreased; the 2.5 percent drop was attributed to new employees, extensive training, and new procedures for SSI (SSA 1974b, 3).
In addition to SSI, the 1972 amendments included changes to other SSA programs. Changes to Medicare entitlement rules prompted SSA in 1973 to mail out 1.7 million notices to disabled individuals and contact some 250,000 uninsured individuals regarding an opportunity to file for Medicare premium HI.9 SSA alerted another 500,000 individuals to a new opportunity to enroll in SMI. The legislation also established procedures to enroll nonbeneficiaries suffering from end-stage renal disease in Medicare (SSA 1973b, 28). SSA field offices enrolled approximately 9,000 individuals into premium HI in FY 1974 (SSA 1974b, 30).
DI claims also increased by 23.1 percent in FY 1974. Pending claims at field offices were up 86.5 percent, DDS claims went up 53.9 percent, and BDI workloads increased 40.2 percent (House Ways and Means Committee 1975, 23). By the mid-1970s, the disability determination process was under enormous strain. Caseloads were extremely large in all states, delays were lengthy, and both were growing. Centrally issued instructional material was out of date—local offices and DDSs frequently found it necessary to improvise local supplements to the official instructional material (Derthick 1990, 39). BDI was again overwhelmed. In just one week in September 1975, and again in April 1976, BDI used more than 16,000 hours of overtime. In September 1976, BDI used over 17,000 hours overtime weekly (McKenna 1976). In response, SSA curtailed "all of the agency's disability activities not absolutely essential to prompt processing of the heavy claims workloads" (House Ways and Means Committee 1975, 6). Once again, SSA deferred its CDR workloads, which would later draw criticism from monitoring authorities.
Appeals of denied claims were also a growing workload. In FY 1972, requests for hearings were filed almost twice as fast as they could be handled. This was partially due to the new BL benefit program and also due to attrition of hearing examiners, who in August 1972 were reclassified as Administrative Law Judges (ALJs) (House Ways and Means Committee 1973, 32). SSA responded by hiring additional ALJs and opening 25 new hearing offices in FY 1973 and approving 3 more offices the next year (SSA 1973b, 11; House Ways and Means Committee 1974, 3). Still, by FY 1975, new hearings backlogs had developed. At a Senate hearing, Commissioner James B. Cardwell stated that bringing the hearings backlog down as quickly as possible was "the most urgent business" of SSA (House Ways and Means Committee 1976, 35).
By June 30, 1976, SSA had reduced pending hearings from 111,169 to 89,769. To accomplish this reduction, SSA
- tested a "model hearing office" to streamline the hearing process and increase support staff responsiveness;
- hired 256 staff attorneys, increasing productivity by 25 percent in affected hearing offices;
- established an Administrative Officer position to serve as an office manager; and
- created a Regional Management Officer in each region (House Ways and Means Committee 1977, 43).
In FY 1977, new hearings requests rose 23 percent, from 157,688 the prior year to 193,657 (SSA 1978a, 64). In response, SSA instituted an "informal remand" procedure, in which local field offices screened new hearing requests based on certain characteristics that experience had shown might lead to an allowance. Field offices forwarded these cases to DDSs for review and possible development instead of to the hearing office (House Ways and Means Committee 1977, 16).
SSA also continued to improve its handling of the SSI workload. In 1978 SSA began electronic exchanges of benefit information with the Veterans Administration, RRB, Civil Service Commission (later the Office of Personnel Management), and DOL to detect cases in which SSI recipients failed to report to SSA any benefits they received from these other agencies. The data exchange with the Veterans Administration alone saved $61 million in annual SSI payments. The agency also began talks with the Department of Defense, IRS, and the states on possible additional data exchanges (SSA 1976, 42; SSA 1978b, 49). SSA would continue to expand its effort to match its computer records with those of federal and state agencies to reduce incorrect SSI program payments over the years. In FY 1990 such matches resulted in estimated program savings of $144 million at a cost of about $35 million (SSA 1991, 10).
Improving Procedural Instructions
Recognizing that the process for delivering instructions to the field had deteriorated, SSA set out to make improvements. In November 1975, SSA began developing a unified Program Operations Manual System (POMS) to replace over 240 separate manuals and handbooks. In late 1978 and in 1979, SSA published the first parts of POMS (SSA 1980a).
From these beginnings in the 1970s came significant advances in later years. In 1989, SSA initiated a pilot project to determine if storing POMS on machine-readable media would be a cost-beneficial alternative to the existing paper system (GAO 1989, 32). This would both eliminate the labor-intensive updates to the paper version and provide an electronic search capability. In 1991, SSA issued its first POMS on CD-ROM. Updates were shipped monthly, but disks were still 6 to 8 weeks out of date when received (SSA 2009b). A GAO report noted that between 1977 and 1993, SSA had implemented over 400 legislative changes to its programs, resulting in "nearly unmanageable" program operational instructions exceeding 40,000 pages (GAO 1993, 13).
The Intranet provided the solution. In 1999, SSA developed a "PolicyNet" site where employees could access all of the agency's program policy and procedural instructions, including POMS. PolicyNet currently provides over 300,000 Web pages of information available at any time. PolicyNet averages 20 million page views monthly from 70,000 unique visitors. SSA publishes over 4,000 updates annually. A PolicyNet Enhancement Project is now under way to make the site even more user-friendly (SSA 2009b).
Processing W-2 Forms: Annual Wage Reporting
Into the early 1970s, SSA's process for posting earnings was not much different from that of the early days. Employers still reported their earnings to IRS via Form 941, Employer's Quarterly Report of Taxable Wages. IRS then sent a record of the wage reports to SSA's BDP, which microfilmed the reports and filed the films for storage and future reference. BDP also entered employer-identifying information onto punched cards and associated it with employee information. Machine-prepared wage reports, including typewritten reports, went to an optical page reader which electronically scanned the employee information and entered it directly onto magnetic tape. Hand-written reports were keypunched. The tapes then entered a computer operation that balanced the wages on each page against the total wage amount reported (SSA 1973a, 5–10; Casey 1977, 25).
On January 2, 1976, P.L. 94-202 instituted an annual wage reporting (AWR) system effective with reports of wages paid in 1978, excluding state employment (SSA 1976, 55). Annual wages were to be gleaned from the W-2 forms, with an accompanying W-3 summary wage report. Employers sent these forms to SSA for processing rather than to IRS. Once processed, SSA sent the wage report information to IRS on a flow basis. IRS and SSA reconciled the wage reports against the quarterly 941 forms, which employers still filed to pay their quarterly payroll taxes. IRS investigated discrepancies associated with incomplete earnings records.
SSA and IRS agreed to a full-year processing cycle for 1979 and 1980. SSA processed the AWR workload in four locations. Data operating centers (DOCs) in Wilkes-Barre, Albuquerque, and Salinas (California) handled paper reports requiring data entry; BDP's Baltimore facility handled reports filed on magnetic media. For the first time, SSA hired seasonal employees to handle data entry in the DOCs (SSA 1980b, 58).
The switch to AWR brought problems and frustrations for both IRS and SSA. Negotiations between the agencies were hampered by different interpretations of the law based on their differing needs. Equipment problems also complicated AWR. The DOCs' new optical character recognition scanning equipment was not fully operational until March, and the data entry upgrade was not fully operational until June—in both cases, several months later than expected (SSA 1980a).
SSA also had problems controlling the reports. Some were processed twice, resulting in posted earnings of twice the amount actually earned. States were especially prone to double posting as some filed two reports—one under a regular EIN and a second time under a special "69" EIN that state governments used.
It would take years for SSA to straighten out all the problems with AWR. Many of the deficiencies would not be resolved until the Systems Modernization effort in the 1980s. Today, SSA still uses an AWR system.
1980s
The 1980s brought more legislative changes for SSA to implement, beginning with the Disability Amendments of 1980 (discussed below) and the Omnibus Budget Reconciliation Act of 1981, which made major changes to Social Security, SSI, Aid to Families with Dependent Children, and other programs affecting SSA. The changes to the OASDI program included phasing out student payments, stopping young parents' payments when a child reached age 16, limiting the lump-sum death payment, changing the minimum payment, and retaining the earnings test at age 72 through 1982, after which the exempt age would be 70. The legislation also imposed a disability "megacap" offset and introduced a new way of computing SSI payments called retrospective monthly accounting (SSA n.d. b).
Resuming Continuing Disability Reviews (CDRs)
As early as 1964, there were concerns that SSA was continuing to pay disability benefits to some individuals after they were no longer disabled. Although SSA had a CDR process at that time, much of the recurring CDR workload was deferred while resources were focused on processing new initial awards and Black Lung applications. The failure to process CDRs continued when SSA had to turn its attention to new SSI disability claims and the SSI conversion rollback (SSA 1995d).
Other factors also contributed to growth in the disability rolls. In the early 1970s, the reversal rate for those filing for reconsideration of a disability claim denial had risen to 30–40 percent and for hearings to about 50 percent (Maldonado 1978). In addition, prior to SSI, BDI reviewed all disability allowances. With the advent of SSI, a 100-percent review was no longer operationally feasible, and it was reduced to a sample performed in special Claims Review Sections located across the nation (SSA 1995f; SSA 1995g).
In 1976, GAO issued a report declaring that people who were no longer disabled were still receiving benefits and that SSA was not taking action to correct the situation. Then a 1979 GAO report severely criticized SSA for not conducting CDRs (SSA 1995f). Meanwhile, an SSA pilot study in the Atlanta and Kansas City regions showed that a small percentage of disability beneficiaries aged 45 or younger in 1979 and first entitled to benefits before 1960 were no longer disabled. Because of this study and the GAO reports, SSA selected a random sample of DI beneficiaries for CDRs to assess criteria for establishing diaries, assumptions about the probability of medical improvement and return to work, and the accuracy of monthly disability payments. SSA ceased working its scheduled CDRs in early 1979 but planned to resume them in 1980 (SSA 1980a).
The Disability Amendments of 1980 and the Omnibus Budget Reconciliation Act of 1981 contained 30 new provisions affecting SSA, one of which required reviewing disability cases. The 1980 amendments directed SSA to commence CDRs on January 1, 1982, and required all cases subject to review to be reviewed every 3 years (Derthick 1990, 75). The law also required SSA to review at least 15 percent of favorable DI determinations on a preeffectuation basis during FY 1981, then 35 percent in FY 1982, and 85 percent from FY 1983 forward (SSA 1982a, 6).
SSA decided to start the reviews early in order to maximize savings and to spread the heavy workload over a longer period (Derthick 1990, 86). These CDRs were "de novo reviews," in effect reopening the initial decision of whether an individual's impairment met the SSA criteria for disability entitlement (SSA 1995d).
SSA funded a substantial increase in state DDS staffing to complete these reviews. To maximize program savings, SSA developed profiles of those most likely to no longer meet the law's definition of disability, and reviewed those cases first. Beginning March 1981, the agency released 30,000 cases each month to the state DDSs. As of May 1982, more than 30 percent of the profiled beneficiaries were determined to no longer be disabled. SSA notified these people that their benefits were terminating. In FY 1982, DDSs conducted 463,008 reviews and issued decisions in 410,496 cases, finding that 45 percent of the reviewed beneficiaries were not disabled (SSA 1982a, 6; SSA 1983, 6).
Despite expectations that the benefit cessations would be high, the 45-percent rate caused great congressional and public concern. Many Congressmen, the public, and the media considered the rate too high and questioned the accuracy of the review determinations. In response, SSA Commissioner John A. (Jack) Svahn announced in September 1982 that field offices would begin face-to-face beneficiary interviews on CDR cases so that interviewers could better explain the purpose of the review. SSA required the DDSs to provide more detail in their disability determination notices and to obtain all existing medical evidence for the 12 months preceding the review. SSA also doubled the number of cases reviewed (SSA 1983, 6–7; SSA n.d. b).
People with mental impairments, which are challenging to evaluate, were particularly affected by the high termination rates (SSA 1995f). Determinations of disability termination were retroactive, sometimes for as many as 15 years. Unfortunately, these terminations coincided with a White House emphasis on debt collection by all federal agencies. Collecting disability payments that were now deemed erroneous from former beneficiaries became a major piece of SSA's debt management initiative. SSA issued overpayment notices asking for repayment of huge sums of money to people with a history of mental impairments who were no longer receiving a monthly check. A few of these individuals committed suicide, and these tragedies were widely reported on newspaper front pages (SSA 1995f).
Naturally, appeals of the termination determinations were high. Hearings increased rapidly, with a record high of 281,737 in 1981. Pending hearings were soon up 17.4 percent over 1980 and were expected to rise even more in 1982 and 1983. SSA made plans to hire an additional 100 ALJs in FY 1983 and to increase the ratio of support staff to ALJs from 4.5:1 to 5:1. SSA also recognized the need to improve the quality and consistency of the decision process between the hearing offices and the state DDSs (SSA 1982a, 6).
Resistance to SSA's de novo decision process on CDRs built rapidly. SSA's field organization tried to persuade headquarters that holding beneficiaries liable for mistakes SSA had made years earlier in its disability process was not sound policy. The DDSs joined the protest. Eventually, 23 governors declared moratoria on processing CDRs in their states (SSA 1995g). In January 1983, Congress also took action to help beneficiaries whose disability benefits were terminated; P.L. 97-455 permitted, on a temporary basis, beneficiaries contesting the termination of their benefits to have both their benefits and Medicare coverage continued through the hearing phase (SSA n.d. b).
By the end of 1984, all circuits of the U.S. Court system, led by a Ninth Circuit ruling, had ruled that SSA must apply some form of medical improvement standards or a presumption of continuing disability before benefits could be terminated. The Ninth Circuit gave SSA 60 days to mail notices advising all of the nearly 29,000 persons in the circuit's jurisdiction who had been terminated without a finding of medical improvement that they could reapply for benefits (Derthick 1990, 140).
Eventually, the Secretary of Health and Human Services (HHS, as HEW had been renamed in May 1980) instituted a moratorium on additional CDRs. SSA had been conducting between 400,000 and 500,000 scheduled CDRs per year; now the agency conducted CDRs only for individuals who returned to work or reported that their condition had improved (SSA 1995g).
The Disability Benefits Reform Act of 1984 provided that SSA could terminate disability payments only if an individual's impairment had improved. It also mandated SSA to develop new mental health regulations more congruent with current mental health standards and practices (SSA 1995f). SSA established a CDR Task Force to formulate plans for reinstating CDR reviews under the provisions of the 1984 legislation. The task force came up with a plan to prioritize the CDRs based on the likelihood of medical improvement. SSA contracted with the American Psychiatric Association to help rewrite the mental health regulations. After publishing a medical improvement review standard as required by legislation, SSA resumed CDR processing in January 1986. DDSs conducted over 400,000 CDRs in 1988 (SSA 1988, 13). On June 30, 1987, SSA established a Federal DDS at its Baltimore headquarters to serve as a test-bed for changes to disability policies and procedures and to help process high-priority disability workloads such as CDRs.
In the ensuing years, SSA would submit an annual budget request for the funds needed to conduct CDRs, and every year the White House would cut most of the CDR funding out of the budget proposal. SSA did not receive money targeted for CDRs for several years (SSA 1987, 11; SSA 1995f; SSA 1995g). Predictably, the CDR backlog grew during this period. SSA performed fewer than 100,000 CDRs annually, and was criticized for not meeting its stewardship responsibilities.
Although costs are incurred to process CDRs, SSA estimates that every dollar spent yields at least $10 in lifetime program savings (SSA 2009e, 19). In the aftermath of events of the 1980s, Congress adopted a 7-year plan in 1996 to eliminate the CDR backlog and increased CDR spending caps for FY 1996–2002. With this funding, SSA eliminated the CDR backlog for DI cases by the end of FY 2000 and for SSI cases by the end of FY 2002. The 7-year plan also called for streamlining the CDR process (SSA 2002b, 4). However, Congress discontinued the extra funding in 2004 (Rust 2008) and the backlog of pending CDRs once again began climbing.
Enumerating Children
The Tax Reform Act of 1986 required taxpayers to have an SSN for each dependent aged 5 or older claimed on tax returns due after December 31, 1987. As a result, SSA expected its typical annual output of 6 million original SSNs to increase to 9 million during 1987 (SSA 1987). Seizing the challenge, SSA contacted 130,000 schools with 44 million students to solicit applications for SSNs. From October 1986 until May 1988, SSA assigned original numbers to almost 10 million dependents aged 5 to 18 and issued over 7 million replacement Social Security cards (SSA 1988).
So that most future requests for SSNs for children would not require field office visits, SSA devised an automated process called Enumeration at Birth. In a three-state pilot beginning August 1987, the parent of a newborn could request an SSN as part of the State's birth registration process (SSA 1988, 2). Additional states began to participate in July 1988. By the end of 1991, 45 states, the District of Columbia, Puerto Rico, and New York City had signed participation agreements (Long 1993, 83). Today, all states participate, and SSA receives nearly three-quarters of all original SSN applications, and 96 percent of original SSN applications for newborns, through Enumeration at Birth. About 4 million SSNs are now assigned through the process each year (SSA 2009l).
Creating a Systems Modernization Plan
During the 1970s, SSA's computer technology deteriorated for a number of reasons. GAO, the General Services Administration, and the Office of Management and Budget pointed out deficiencies in SSA's computer system resulting from long-standing systems planning, management, and operational weaknesses (SSA 1982b, 4).
The system was "held together with rubber bands and chewing gum—cast-off equipment" (SSA 1995e). SSA was buying used computers just to keep operating (SSA 1995h). In 1978, SSA's newest computer was 14 years old. The agency's large-scale production computers were so antiquated that not a single model was still marketed by the manufacturers. Replacement parts were not guaranteed, and maintenance costs were high. SSA missed processing deadlines regularly, even with the machines operating 24 hours a day, 7 days a week. Telecommunications workloads were projected to far exceed the capacity to handle them (SSA 1986, 10).
By the early 1980s, the SSA Data Acquisition and Response System (SSADARS), the network that linked SSA's field facilities with the agency's new National Computer Center via intermediate concentrators in the 6 PSCs and within the Center itself, was handling about 850,000 transactions daily. A second telecommunications system, the Batch Data Transmission system, exchanged batched information between the National Computer Center and several remote sites, such as the PSCs, the DOCs, RRB, Treasury Department, Medicare carriers and intermediaries, and several state welfare agencies. SSADARS and the Batch Data Transmission system facilities could not exchange information with one another. In addition, SSA had several smaller specialized networks. Many of these systems and the telecommunications lines were plagued with problems, outmoded, or of insufficient capacity (SSA 1986, 16).
Inadequate funding was a major factor in the sad state of SSA technology. According to a former SSA executive, the Chair of the House Government Operations Committee, Jack Brooks (D–TX), froze SSA's procurements and refused to allow the agency to buy any technology infrastructure that was not purchased on the open market—even if it would not support any of SSA's existing software applications, and would require SSA to rewrite all of its software to run on it (the cost of which SSA could not consider in its request) (SSA 1995h).
It's not that SSA's software didn't need rewriting; it was just impossible to rewrite it quickly enough to run on a completely new platform. In 1980, SSA's automated data processing operations comprised 76 different software systems consisting of 1,376 computer programs with over 12 million lines of undocumented instructions written in low-level computer languages (SSA 1986, 6).
In its Annual Report to Congress for FY 1981, SSA cited modernizing its data processing systems as its top priority. The agency had drawn up a 5-year modernization plan to replace its outdated system of hardware, software, and storage capacity. The plan included four programs: software engineering, database integration, capacity upgrade, and a data communications utility to replace SSADARS. The cost of moving from "survival mode" to a modern system in 5 years was estimated at $479 million (SSA 1982b, 5). In March 1982, SSA published its Systems Modernization Plan: From Survival to State of the Art. To develop the plan, a team of 35 SSA analysts interviewed over 200 managers and their employees to learn the agency's business processes and its information and computer support requirements. The team also inventoried current system capabilities (SSA 1986, 6).
To procure systems modernization funding, Commissioner Svahn candidly disclosed the critical state of SSA's systems. On Capitol Hill and in the media, Svahn stated that SSA's system was on the verge of collapse, and that timely distribution of benefit checks was at risk. At an April 1983 hearing on SSA systems modernization, Representative J.J. Pickle (D–TX) pointed out that one of the largest companies in his district had 12,000 employees whose earnings had not been posted. Svahn opportunely observed that SSA's computers were on the brink of failing. When the commissioner requested the $479 million needed for support systems modernization, Congress concurred (SSA 1995d; SSA 1995h).
In the meantime, SSA had migrated many of its data processing operations to a new National Computer Center in 1982, consolidating and reconfiguring existing mainframe processors as part of the move. Also in 1982, SSA acquired two modern large-scale host processors to replace the outdated processors used for data communications. Additionally, SSA installed a new large-scale processor dedicated solely to modernization activities (SSA 1982b, 3). In 1984, SSA replaced the eight old, low-capacity computers that supported its programmatic workload with four new large-scale mainframes, one of which was used for a program testing network (SSA 1986, 10). By 1990, the National Computer Center had 14 major mainframes supporting a database of 1.3 terabytes, processing about 453 million instructions per second and about 7 million online transactions daily (National Research Council 1990, 2).
Another modernization was the conversion, beginning in 1982, from magnetic tape to direct-access storage devices for the enormous amounts of data the agency collected. At its zenith, SSA's tape library contained nearly 700,000 reels—enough magnetic tape to stretch to the moon and one-third of the way back. Mounting the tapes was very labor intensive. Also, storing the master file records on tape did not support online data retrieval; SSA was creating a duplicate of the master files for operational employees to query (SSA 1986, 21). Direct-access devices, on the other hand, could be queried directly. SSA initially acquired 282 billion characters of high-density disk storage (SSA 1982b, 2), but this soon proved to be not nearly enough. By 1986, SSA had acquired 360 disk drive units with 780 billion characters of storage capacity to house all of SSA's master files and most intermediate files. Backups, and some active files, were still maintained on 250,000 reels of tape (SSA 1986, 22).
As part of Systems Modernization Plan software improvements, SSA set out to modernize its four major business processes: SSN enumeration, annual wage reporting, claims (both OASDI and SSI), and postentitlement workloads (particularly debt management). It also developed software life cycle development standards and methodologies using top-down requirements analysis for these four processes.
In March 1984, SSA put together a team of executives from the critical components—the Offices of Systems, Operations, Program Policy, and Management—to act as a steering committee for the Claims Modernization Project/Field Office Systems Enhancement (CMP/FOSE) project. The Office of Systems set up a Model District Office in the Baltimore headquarters, and the Office of Operations brought in field office employees from across the country to participate in testing the new software system. A model PSC called the Test Processing Module soon followed (Willeford 1985).
CMP/FOSE had multiple aspects. The software initiative produced the Modernized Claims System (MCS), which enabled representatives to enter claims data directly during an interview. Initially, the data passed to the existing Claims Automated Processing System; by 1990, the data were passed into a completely new back-end processing system. MCS eliminated the need to transfer the paper application information to a computer coding form and then for a teletypist to input the code. MCS also provided online interfaces with some of SSA's databases, for purposes such as checking that the name and SSN matched. MCS also provided a Workload Management System (WMS) to keep track of pending claims and produce management information. Until this time, field offices kept track of claims with the same kind of Flexoline strips that the Bureau had used in 1937 to keep track of SSNs issued (Willeford 1985).
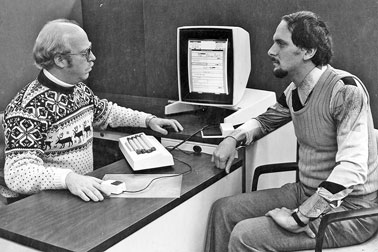
OASIS photo.
The hardware component of CMP/FOSE was the Terminal Acquisition Project (TAP). The MCS computer-based application intake required that all field office interviewers be equipped with computer terminals, both at their desks and in special "front-end interviewing" areas set up in some offices in order to increase the privacy of interviews and to protect the confidentiality of beneficiary information. The TAP terminals were "dumb," having no central processing unit; rather, they transferred data via the concentrators to the mainframes in the National Computer Center for processing. Employees could use the terminals not only to take claims, but also to query online databases for prior claims data or to request an online benefit estimate (Willeford 1985).
Support staff such as receptionists, clerical workers, and data review technicians also required computer terminals to assist in claims development and processing. Anticipating resistance from budget monitoring authorities, SSA kept its terminal procurement request low and required support staff to share terminals. However, with all claims information online, this proved to be unworkable. The PSCs and the Office of Disability Operations also needed TAP terminals, both to view the online screens for processing claims for which the field offices could not trigger payments and to process adjustments to payments (Willeford 1985). By FY 1987, SSA was installing about 1,000 terminals per month. By FY 1988, SSA had installed about 25,500 TAP terminals nationwide (SSA 1988, 17; National Research Council 1990, 13).
Sites for training instructors on the new online claims system also required terminals. Training was a major undertaking. How could SSA give its entire direct-service staff a 2-week training program without closing an office or hindering service delivery? The answer was to use a train-the-trainer approach. Two employees from each region attended a training class on the new hardware and software in Baltimore. These employees then returned to regional training sites, where they trained two employees from each local office. SSA created a "training region" on its mainframe with an MCS mockup on which employees could practice inputting claims interview information. This was a tremendous aid in training the trainers who fanned out to the 1,400 operational sites to train operational employees. To maintain service to beneficiaries and applicants, an office would train only half of its employees at a time. Also, other field offices would assume responsibility for the office's initial OASDI claims during training (Willeford 1985).
To support the additional terminals, all 1,400 office facilities had to be modified to provide additional space, cooling, data circuits, and cabling. SSA undertook a related effort to install ergonomic, modular furniture and ergonomic chairs in operational offices.
For the first implementation stage, the Office of Operations selected the downtown Baltimore and the York, Pennsylvania field offices to pilot the new software and hardware. SSA also set up pilot processing modules, one in the Office of Disability Operations in Woodlawn, Maryland, and the other in the Mid-Atlantic PSC in Philadelphia (SSA 1985a, 14). These two modules would service most claims taken by the pilot field offices. On March 20, 1985, according to a schedule made 2 years earlier, SSA took its first claim using MCS in the York office. By early 1986, 20 pilot field offices (2 in each region) and SSA's 8 claims processing centers were handling claims via the new system. At the start of 1987, the first national implementation site, the M Street District Office in Washington, D.C., began processing claims under the new system. By spring 1987, more that 200 field offices were using MCS (SSA 1987, 7). National MCS rollout was complete in 1988.
Undergoing Staff Reductions
Having campaigned on a platform opposing big government, President Ronald Reagan took steps to reduce the size of the federal workforce in the 1980s. For SSA, this translated into a reduction of 17,000 employees over 6 years beginning in 1984—a loss of 1 out of every 4 employees. Reportedly, the Reagan administration had wanted even larger SSA staff cuts (SSA 1996a). In response, SSA instituted a hiring freeze and shrank from 81,532 employees in 1984 to 66,000 by the end of 1988, during which the operational workloads increased 12.4 percent. As a result, postentitlement review workloads were backlogged both in field offices and the PSCs (National Research Council 1990, 16).
By using attrition to reduce its numbers, SSA created staffing imbalances. In January 1987, SSA implemented a plan to redeploy employees from its headquarters and regional offices to the direct-service operational components, such as field offices, where they were needed to process work (SSA 1988, 8). However, in 1989 GAO reported that these efforts were only minimally effective and "in the absence of a comprehensive work-force plan, staffing imbalances occurred, which led to inefficient operations and ad hoc stop-gap measures to relieve problems" (GAO 1989, 25).
Phoning in for Service, Part I
SSA's difficulties in processing its postentitlement workloads were complicated by efforts to implement a toll-free phone service that coincided with the staff cuts. In 1987, SSA's toll-free service consisted of 34 local sites working independently. On October 1, 1988, SSA launched the National 800 Number Network to assist the agency in handling both nationwide general inquiries from the public and postentitlement reports from beneficiaries.
SSA created its National 800 Number Network by integrating the existing 34 local sites with three new teleservice centers in Birmingham, Honolulu, and San Juan. To oversee the new national network, SSA established an 800 Number Control Center in Baltimore. The control center manually balanced call loads coming into the network among the sites that were open. At the startup, the National 800 Number Network provided service to 60 percent of the country, comprising the 50 percent of the public previously covered by the local teleservice centers plus an additional 10 percent of the population who previously paid toll charges to reach SSA offices. The new 800 number service was available each weekday from 7 a.m. to 7 p.m. Initially, automated telephone response units also allowed callers to leave open-ended messages when the call center was closed, to which agents could respond later.
On October 1, 1989, SSA extended 800-number service to all U.S. callers. To help with the additional call volumes, SSA folded some smaller sites into larger ones and opened "mega sites" in Albuquerque, Auburn (Washington), Baltimore, and Birmingham. There were now 36 call center sites, ranging in size from 20 to 500 employees. As with any new venture, the National 800 Number Network suffered some growing pains, and heavy call volumes resulted in high busy signal rates. To help alleviate call congestion, callers were offered telephone response unit service as an alternative to talking to an agent.
SSA's field offices had been taking initial claims over the phone for many years. In FY 1987, SSA expanded this practice to allow teleservice centers to schedule teleclaims for the field offices (SSA 1987, 5). By FY 1988, SSA was taking about half of its claims via telephone. The agency also began to offer appointments for face-to-face field office interviews scheduled via calls to the 800 number or field office (SSA 1988, 6). In 1998, in an effort to help callers file retirement and survivor claims by phone, SSA would pilot "immediate claims-taking units" at several existing call answering sites; full rollout followed in 2000.
1990s
On March 31, 1995, in a ceremony at its Baltimore Headquarters, SSA once again became an independent agency. On December 14, 1999, the Foster Care Independence Act added a new program for SSA to administer under Title VIII of the Social Security Act. This program provided cash benefits for certain World War II veterans, particularly Filipino veterans. Nevertheless, the agency's primary challenges during the decade would continue to involve SSI and the disability process.
Complying with Sullivan v. Zebley
In its February 20, 1990, decision on Sullivan v. Zebley, a nationwide class action suit, the U.S. Supreme Court held that substantial parts of the SSI regulation on determining disability for children were inconsistent with the Social Security Act. In making a disability decision for an adult, SSA considered not only the impairment but also the applicant's vocational history. As children have no vocational history, SSA had decided in 1973 to prepare special Listings of Impairments for children and to decide each child disability case on the basis of the medical issues alone. In Zebley, the Court ruled that by requiring children to meet or equal SSA's Listing of Impairments alone, the agency failed to consider the functional impact of children's impairments, and that SSA should have considered a child's ability to do age-appropriate activities in making its disability determinations (SSA 1991, 22; SSA 1995g).
To comply with Zebley, SSA was required to reopen every SSI children's disability denial back to 1980. SSA expected to have to readjudicate about 550,000 retroactive claims, along with an ongoing workload of 135,000 additional cases per year under the new standards (SSA 1991, 26). SSA's Commissioner established an intercomponent work group to implement the Zebley decision. Normally, SSA would have to publish new regulations in the Federal Register, request public comments, and wait for the comments before applying the revisions and reevaluating the cases. As this process was expected to take a year, SSA developed an interim standard so as to immediately begin reevaluating cases that were expected to meet the new requirements. SSA processed about 150,000 cases under the interim standard while working on the new regulation (SSA 1995g).
SSA took the Zebley ruling as an opportunity to consider other changes in the childhood disability criteria. SSA assembled childhood and pediatric experts to help develop the best criteria for evaluating children. One of the recommendations was an "individualized functional assessment" that focused on behavioral problems as a type of disorder (SSA 1995g).
After soliciting public comments, SSA published the revised final rules for determining disability in children in 1993. These new standards included
- a new step to determine if a child's impairment had more than a minimal effect on his or her ability to function (equivalent to the severity step found in the adult rules),
- a new approach to satisfying the Listing of Impairments for children, called "functional equivalence," and
- an Individualized Functional Assessment for evaluating a child's impairment beyond the medical listings to parallel the vocational steps applied in adult cases and to satisfy the "comparable severity" criterion (Harmon and others 2000).
SSA worked with 150 national organizations to reach approximately 450,000 children whose claims might be affected by the court decision. The agency also placed more than 125,000 posters in English and Spanish in offices of state and local government agencies and nonprofit organizations that provided services to disabled children (SSA 1992a, 20).
SSA processed the readjudications over a period of just over 3 years. Before Zebley, SSA's allowance rate for children at the initial claim level was about 40 percent, somewhat higher than the adult rate. Immediately after implementing the new standard, the rate increased to 50–60 percent. Also, because of increased public awareness and agency outreach, the number of children applying for SSI disability tripled, to about 250,000 cases per year. Between 1990 and 1996, the number of SSI child recipients increased from about 350,000 to more than 965,000.
Meanwhile, allegations began to surface that all a child had to do was misbehave in the classroom and SSA would approve the child for SSI payments. Although SSA studies did not support this allegation, the press picked up anecdotal accounts of supposed abuses of the program. National news reports featured stories of "crazy checks" and of children being coached by parents to misbehave in order to qualify for SSI (SSA 1995g; Harmon and others 2000).
In August 1994, the Social Security Independence and Program Improvements Act established a National Commission on Childhood Disability to review the new SSI definition of childhood disability and related issues. The commission's final report in November 1995 contained several recommendations for strengthening the SSI childhood disability program, but no unanimity on whether the definition of disability should be changed. During this period, GAO issued two reports on the post-Zebley childhood disability rules, and the National Academy of Social Insurance published a "Report of the Committee on Childhood Disability, Restructuring the SSI Disability Program for Children and Adolescents" in January 1996 (Harmon and others 2000).
Congress responded to the child disability determination controversy by passing new standards as part of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996, commonly known as the "Welfare Reform" legislation. This legislation eliminated the "comparable severity standard" and the reference to "maladaptive behavior" in the childhood standards. Instead, the new standard provided that a child is considered disabled only if he or she "has a medically determinable physical or mental impairment which results in marked and severe functional limitations." Congress required SSA to review the decisions made on childhood disability claims under the post-Zebley standards within 1 year of enactment and to remove children from the rolls if they could not qualify under the new legislatively mandated standards. Congress also required that SSA reevaluate each SSI child's eligibility under adult disability standards within 1 year of the child attaining age 18 (SSA n.d. b; Harmon and others 2000).
SSA had to identify and then notify the families of children potentially affected by the legislation, who accounted for approximately 288,000 of the 1 million children receiving SSI disability payments. It took until February 1997 for SSA to issue new SSI childhood disability regulations complying with the Welfare Reform legislation. As implementation of the new standards began, SSA identified three areas of concern: the status of children classified with mental retardation, variations among states and categories of impairments in the accuracy of decisions to continue or deny payments, and allegedly difficult-to-understand notices causing confusion about appeal rights (SSA 1997b).
As promised at his 1997 confirmation hearings, new SSA Commissioner Kenneth Apfel's first act was to order a comprehensive review of SSA's implementation of the new childhood provisions. His primary concern was to see if the provisions affecting the childhood disability rules had been implemented fairly and to inform the public, Congress, and the president of his findings (Harmon and others 2000). Commissioner Apfel announced the results of his "top to bottom" review of the SSI childhood disability determination process on December 17, 1997. By this time, SSA had completed eligibility redeterminations of about 263,000 of the 288,000 SSI children subject to review under the provisions of the Welfare Reform law. While expressing overall confidence in the quality of the disability determinations, Apfel acknowledged that some problems were found. The Commissioner directed a new review of approximately 45,000 of the 135,000 cases in which payments had ceased. For those whose payments had ceased and who had not appealed, a second appeal opportunity was offered. In addition, all 15,000 new claims filed since the August 1996 passage of the Welfare Reform changes in the law were to be reviewed again (SSA n.d. b).
On February 18, 1998, SSA sent notices to 86,000 families whose children lost SSI eligibility under the Welfare Reform law. The notices provided a second opportunity to request either an appeal or payment continuation during appeal. Responding to this examination and reexamination of the criteria for finding children eligible for SSI disability payments, SSA once more published revised regulations, now effective January 2, 2001. These rules clarified and expanded factors that had to be considered in evaluating childhood disability and simplified and revised the functional equivalence rules (Harmon and others 2000).
Reassessing SSI for Noncitizens
For SSA, the 1996 Welfare Reform legislation meant not only a change in the definition of SSI childhood disability but also changes in the SSI eligibility of most noncitizens. Both changes were problematic and required many years of working closely with the advocacy community to agree on implementing regulations and program instructions. Once again, Congress would rethink its initial legislation and change the rules multiple times (Harmon and others 2000).
Prior to the August 1996 legislation, to be eligible for SSI an individual had to be a U.S. citizen or national, a noncitizen lawfully admitted for permanent residence, or a noncitizen who was a permanent resident under color of law. "Permanent resident under color of law" was not a specific immigration status but a court-defined collection of 17 statuses plus a general category that included any noncitizen residing in the United States with the knowledge and permission of the Immigration and Naturalization Service (INS), against whom INS was not taking action to deport. Thus, except for temporary visitors such as students and undocumented noncitizens, most disabled noncitizens legally in the United States could become eligible for SSI if they met the other SSI program requirements (Harmon and others 2000).
As the United States sought to trim the welfare rolls, the SSI eligibility of noncitizens began to be reconsidered. In 1995, GAO reported that the number of legal immigrants in the SSI program had increased dramatically. In 1982, 6 percent of aged SSI recipients were immigrants, but by 1993 immigrants represented 28 percent of aged SSI recipients. Among disabled SSI recipients, the share who were immigrants had increased from 2 percent to 6 percent. GAO predicted that if the trend continued, the number of immigrants on SSI could reach nearly 2 million by 2000 (Harmon and others 2000).
To reduce these numbers, the Welfare Reform legislation tightened the eligibility criteria for noncitizens. As of the date of enactment, no new noncitizens could be added to the SSI recipient rolls, and all existing noncitizen recipients would be removed from the rolls as of August 1997 unless they met one of the exceptions in the law. To restate a rather complex requirement in simpler terms: To qualify for SSI, not only would a noncitizen have to be a "qualified noncitizen" (a lawful permanent resident or military veteran), the immigrant (or the immigrant's spouse or parent) also would have to have 40 qualifying quarters (earnings credits) under Social Security. In addition, noncitizens who were granted refugee status or similar humanitarian immigration classifications were limited to 5 years of eligibility, unless they obtained citizenship before the 5 years elapsed (Harmon and others 2000; SSA n.d. b; SSA 2009a, 24).
On February 3, 1997, SSA began mailing notices (including an INS fact sheet on citizenship) to approximately 900,000 noncitizens whose SSI eligibility might be affected by the new criteria. SSA estimated that about 500,000 of these individuals would lose their SSI eligibility (SSA n.d. b). Upon release of the notices, SSA field offices were inundated with distraught noncitizen SSI recipients. Many of the immigrants had been in the United States for many years and had no relatives or other means of support if their SSI payments were to end. SSA took steps to help those who might lose their payments. SSA and INS matched computer records to double-check immigration status so that individuals would not be inadvertently suspended. SSA also set up six "mega-sites" in areas of large noncitizen populations to provide noncitizens with information and to help them obtain proof of their immigration status (Harmon and others 2000).
SSA's Acting Commissioner, John B. Callahan, began visiting SSA field offices, community centers, and other gatherings of noncitizens to listen to their stories and to assure them that the Clinton Administration was doing everything possible to make sure that individuals would not lose their SSI eligibility. SSA also worked closely with immigration advocacy groups, states, and local government agencies to assist the immigrants. The situation was dire enough that President Bill Clinton mentioned his concern about the noncitizens' SSI provisions in his 1997 State of the Union address (Harmon and others 2000).
As a result of negotiations between the administration and Congress, the Balanced Budget Act of 1997 included provisions to restore SSI eligibility for all disabled legal immigrants who were or became disabled and who entered the United States prior to August 23, 1996. It also extended for up to 1 year the period for redetermining the eligibility of certain noncitizens who might ultimately not be eligible for continued payments. In addition, the law extended the period within which refugees and individuals in similar humanitarian immigration classifications had to obtain citizenship from 5 years to 7 years, and added Cuban and Haitian entrants and Amerasians to the categories of noncitizens who could be eligible for SSI for 7 years (SSA n.d. b; Harmon and others 2000).
The Balanced Budget Act of 1997 continued SSI eligibility for nearly 300,000 noncitizens who were receiving SSI as of August 5 and restored potential SSI eligibility for an estimated 75,000 individuals who were lawfully residing in the United States on August 21,1996, but who had not filed for SSI before then. However, one group of noncitizen SSI recipients was still at risk of losing eligibility because they were not "qualified." There is no single defining characteristic that identifies this group; they are simply those who, for one reason or another, fell between the cracks of the definition of qualified noncitizens. The legislation extended their eligibility until September 30, 1998 (Harmon and others 2000).
As the date that these noncitizens would lose their SSI payments approached, a concern arose that SSA's records might not have accurately reflected the current immigration status of some of the individuals. Although SSA had notified all noncitizens on the SSI rolls several times about the changes in the law and urged them to contact their local SSA office, some recipients did not do so. SSA conducted a statistically valid sample survey in 1998 to determine the extent to which SSI records of the "nonqualified" noncitizens accurately reflected their current citizenship or immigration status. The study found that a large percentage of the "nonqualified" noncitizens actually were in an immigration category that would have qualified them, but for a number of reasons, they had not contacted SSA. SSA sent the study results to congressional staff and convinced the appropriate members of Congress to also "grandfather in" nonqualified noncitizens who had received SSI prior to the enactment of the Welfare Reform Act. The Noncitizen Benefit Clarification and Other Technical Amendments Act of October 1998 permanently extended SSI eligibility to the remaining "nonqualified noncitizens" who were receiving benefits in August 1996 (Harmon and others 2000).
Since the 1990s, a number of additional legislative acts have further modified the provisions for SSI eligibility of noncitizens and have extended the period of eligibility for humanitarian immigrants. Recent legislation has extended benefits to Iraqi or Afghan nationals who served the U.S. government or who acted as translators or interpreters for U.S. armed forces in these countries.
Phoning in for Service, Part II
In FY 1990, SSA teleservice centers received approximately 53 million calls that were answered by 3,500 representatives (SSA 1991, 10). The service goal for 1991 was modest: All customers would get through to SSA within 24 hours. SSA continued to improve its 800-number service throughout the 1990s, changing how calls were handled and adding new technology to the National 800 Number Network. Improvements included expanding bilingual service to Spanish-speaking callers nationwide and extending service to other languages via an interpreter service. SSA also expanded service for users of Telephone Device for the Deaf systems. Routing changes allowed calls to be sent to the next available agent anywhere in the nation, and improved forecasting tools helped the agency better meet increasing demands for service. SSA also developed the Customer Help and Information Program, a decision-support system to help agents handle calls correctly and consistently.
By 1994, SSA's service goal was to enable callers to get through within 5 minutes, but demand was still growing; by 1997 demand was so great that for several months the busy signal rate reached 50 percent (GAO 1997, 11). SSA responded by enhancing its network technology and by simplifying the process to allow more calls to be handled at the first point of contact. SSA also looked for more staff to answer the phones. Office of Central Operations employees and PSC employees who handled postentitlement actions were tapped to answer the 800-number calls during spike periods. However, time spent answering the phone was time that these "spike" employees took from processing their traditional workloads. The result was an increase in backlogs in maintaining beneficiary records and making timely payment changes even as employees increased overtime hours (GAO 1997).
By 1999, even though calls numbered nearly 60 million, SSA was meeting its goal of answering 95 percent of its calls within 5 minutes. Seventy-five percent of callers reported that their transaction was completed on the first call, and 90 percent were pleased with the agent's courtesy. A quality assessment report showed 95 percent accuracy for answers to questions on payments. However, 3,200 PSC and Office of Central Operations "spike" employees still handled 24.6 percent of the calls, resulting in growing postentitlement backlogs. The access goal of 95 percent of callers getting through within 5 minutes was lowered to 92 percent, as SSA simply lacked the staff numbers to maintain the higher target (Apfel 2000).
As the new millennium arrived, the demand for National 800 Number Network services steadily grew. SSA offered several additional automated services, allowing callers secure access to personal data. Many automated services offered an interactive speech format, enabling callers to provide more information to SSA. To make better use of callers' time while they waited to speak with an agent, SSA instituted "screen pop" and "screen splash" applications to collect data from callers and match the information to SSA records. In 2008, SSA also added "scheduled voice callback" to the National 800 Number Network, allowing a caller to leave his or her phone number, hang up, and receive an agency callback within a specified time when the network was less busy. The public response to this application has been very favorable.
Today, the National 800 Number Network receives over 82 million calls and handles 67 million transactions a year through agents and automated services. The contributions of over 6,500 teleservice agents have enabled the agency to consistently meet the established goals for caller access and speed of answer. In 2009, the average time to answer calls was just 245 seconds, and the average busy signal rate was down to 8 percent (Astrue 2009).
For its timely and exemplary performance the National 800 Number Network has received several awards, including the Federal Executive Board Award for Innovation in Public Service. The Network has also been rated by Dalbar Financial Services, Inc.—a provider of market research on customer service—as the best 800 number in the nation for courteous, knowledgeable, and efficient service.
2000s
While the Social Security program's future was being discussed in the media, SSA employees went about their day-to-day tasks. By 2000, about 100,000 people visited one of SSA's 1,300 field offices and over 240,000 people called the 800 number each workday. Also, SSA processed an average of 20,000 initial claims and held 2,400 hearings each workday, and processed over 250 million earnings items a year. Postentitlement workloads had grown by almost 25 percent over the previous 10 years, from 80 million to 100 million actions, primarily for program integrity activities such as SSI redeterminations and CDRs. The agency spent $1.7 billion, about one-quarter of its administration budget, on program integrity (Apfel 2000). By 2008, SSA was averaging over 160,000 visitors, processing over 26,500 initial claims, and holding nearly 2,500 hearings per workday (McMahon 2008). In 2009, SSA processed 271 million wage items (SSA 2009e, 7).
During the 2000s, SSA prepared for the onslaught of filings from baby boomers who would begin reaching retirement age in 2008 and had already reached the prime age for claiming disability benefits. At the same time, SSA faced widespread retirements in its own ranks. In 2000, the average age of SSA employees was 46. SSA conducted a "retirement wave" study to predict losses and support workforce planning. Retirements were predicted to peak from 2007 through 2009, causing 4.6 percent staff losses each year. Instead of waiting for the losses to occur, SSA "flattened the wave" with an early retirement program from 1996 through 2000 (Apfel 2000). This program permitted the orderly replacement of older employees with younger ones. In the first half of 2002, SSA was able to hire approximately 18,350 new permanent employees to replace losses (Barnhart 2006).
In 2004, SSA developed its first Human Capital Plan, which is now updated annually. SSA also developed a Future Workforce Transition Plan. SSA's retirement wave appears to have crested in 2007, when 3,074 employees, 5 percent of the workforce, retired. Still, as of October 1, 2008, 24 percent of SSA's employees were eligible to retire, and by 2018 that figure is projected to climb to 50 percent (SSA 2009f).
Improving the Disability Determination Process
The disability determination process underwent major changes in the 2000s. In the 1990s, SSA had identified the need to reexamine its entire disability process. The number of disability claims filed was continuing to rise, and the disability workloads, both DI and SSI, were consuming ever-larger portions of the agency's resources. SSA was having significant difficulty providing satisfactory service to its disability applicants.
In 1965, 97 percent of allowances were decided by the state DDS. By the mid-1970s, 40–50 percent of appealed DDS disallowances were overturned at the hearing level, and by 1980, nearly 60 percent were. Why were so many cases denied at the state level being approved at the hearing level? A number of reasons have been suggested. The passage of time between decision and appeal could have brought the worsening of a chronic medical condition. ALJs frequently had additional evidence not available to the DDSs. DDSs followed program rules, as opposed to ALJs, who depended more directly on the law itself. ALJs had face-to-face contact with the claimants; DDS employees did not. At hearings, about 40 percent of claimants were represented by attorneys. Also, DDSs were under pressure to meet productivity goals.
During the 1990s the Clinton Administration launched an effort to reengineer government under the auspices of the National Partnership for Reinventing Government, also known as the National Performance Review. SSA began to look for processes to streamline in 1993, and targeted disability claims. SSA issued its Plan for a New Disability Claim Process on September 7, 1994 (SSA n.d. b; Harmon and others 2000).
SSA began testing concepts for reengineering the disability process in 1995. GAO conducted several audits of the disability redesign and was generally critical of both the scope of the initiatives and the pace of progress. In response, SSA completed a major reassessment of redesign initiatives in February 1997 that narrowed the focus to the activities most critical to success, including testing process changes, implementing process unification initiatives, and developing long-term support through other enablers. The remainder of the 1994 plan was basically discarded (Harmon and others 2000).
A related 1990s initiative involved the hearing process. Pending workloads in the Office of Hearings and Appeals (today known as the Office of Disability Adjudication and Review) had more than doubled between 1988 and 1995, and average processing times had risen to 200 days. By 1998, the average processing time was up to 365 days (Apfel 2000). SSA tried a number of initiatives to improve the hearing process: a Senior Attorney program, screening units, decision-writing units, case preparation units, a modular disability folder, informal remands to the DDS, and additional automation. Office of Hearings and Appeals staff levels increased 12 percent, from 6,020 employees in FY 1995 to 6,791 in FY 1998. Overtime use in processing hearings increased by 61 percent, from 625,000 hours to over 1 million hours, and other SSA components contributed 2,200 work-years toward hearings from 1997 to 1999. In spite of these efforts, average processing time for a hearing case was 314 days in FY 1999 (Harmon and others 2000). In August 1999, SSA responded to a directive from Commissioner Kenneth Apfel by issuing its Hearing Process Improvement Plan. The plan's goals were to reduce processing times, increase productivity, and provide better overall service to the public (Apfel 2000).
SSA's fourth and final level for deciding claims is the Appeals Council. Claimants who receive an unfavorable decision at a hearing can request an Appeals Council review. In the 1990s, the Appeals Council was also experiencing difficulties. In 2000, SSA released the Appeals Council Process Improvement Plan, which focused on reducing pending workloads and processing times in the short term and on developing an operational structure able to continue delivering high-quality, timely, and efficient case processing for the long term (Apfel 2000).
On November 14, 2001, Jo Anne B. Barnhart was sworn in as the new Commissioner of SSA. The following month, SSA's Inspector General issued a report criticizing the disability process changes, finding that "SSA's initiatives have not resulted in significant improvements to the disability determination process." The agency had failed to meet 10 of its 14 disability-related performance goals for FY 2001—and met none in the hearing and appeals process (SSA 2001a).
In September 2003, Commissioner Barnhart announced a Disability Process Improvement project. Changes included accelerating the transition to electronic recordkeeping, with rollout to begin in January 2004; updating the medical listings of definitions of impairments that SSA finds severe enough for a finding of disability; and improving the hearing and appeals processes (SSA 2003, 16). The agency also established a "Quick Disability Determination" process for DDSs to expedite initial determinations for claimants who are clearly disabled.
The Electronic Disability System (eDIB) is a major initiative that began in the late 1990s and continues today. Its primary objective was to convert all SSA components involved in disability claims adjudication or review to electronic recordkeeping, featuring an "electronic disability folder" that can store digital images of medical records. A web-based application replaced the paper forms that field offices had used to collect information about a claimant's medical and vocational history. As a result, claimants can now enter information themselves via the Internet. Forms that once were printed and signed by hand are now created and stored in the electronic folder and automatically shared with the DDS systems, eliminating rekeying. Files are no longer physically transferred: Any employee involved in processing a case can access the contents of the electronic folder. Hearing offices can also access the information, and are fully integrated into the electronic processing of disability claims (Gerry 2006).
As of January 31, 2006, all 53 state and U.S. territory DDSs had rolled out the electronic disability folder, and more than half were creating and processing all new cases electronically. By 2006, the electronic folder housed over 36.5 million records and was the world's largest repository of electronic medical records (Gerry 2006).
SSA has also begun testing the collection of electronic medical records from health care providers through the Nationwide Health Information Network (NHIN), a system sponsored by the Department of Health and Human Services and supported by several federal agencies. SSA is the first federal agency to exchange electronic medical records via NHIN as part of SSA's Health Information Technology (HIT) project. At a test site in Virginia that began transmitting electronic records via NHIN in early 2009, processing time was significantly reduced. SSA is also using HIT with a Boston facility where an electronic request for a patient's medical records is sent automatically when a patient from this facility files a claim (SSA 2009e, 18; SSA 2009k). On August 7, 2009, SSA announced it was making $24 million from American Recovery and Reinvestment Act funds available in contracts to provide the agency with electronic medical records. The awardees will be required to send electronic medical records to SSA, with a patient's authorization, through NHIN (SSA 2009k). In February 2010, SSA awarded nearly $20 million to 15 entities based on competitive contracts (SSA 2010a).
SSA History Museum & Archives.
However, SSA's efforts to improve the disability process have been hindered by inadequate funding. From FY 2001 through FY 2007, Congress appropriated an annual average of $150 million less than the President requested (Rust 2008). At the same time, workloads continued to grow.
On February 12, 2007, Michael J. Astrue was sworn in as SSA Commissioner. Reducing SSA's growing disability backlogs was his first priority. He quickly reassessed earlier plans to improve the disability process and put his own stamp on SSA's efforts.
From 2001 to 2007, the number of pending hearings had doubled. By May 2007, 738,000 cases were awaiting a hearing decision, and average waiting time was 505 days, the highest in SSA's history (Astrue 2007). Commissioner Astrue directed the agency to focus on processing those claims that had been awaiting a hearing the longest, starting with those pending 1,000 days or more. SSA reduced the number of those cases from 63,700 on October 1, 2006, to 108 by September 30, 2007, and began to work on cases pending 900 days or more (SSA 2007b).
To increase its hearing capacity, SSA also hired additional ALJs, along with support staff to handle the work involved in preparing the cases. Because of litigation and budget cuts, the agency's ALJ workforce by 2008 had declined about 10 percent from a decade earlier, even though the number of cases awaiting a hearing had doubled. During FY 2008, SSA hired 190 new ALJs and eliminated virtually all of the 135,000 cases for aged claimants pending 900 days or more (SSA 2008c). In 2009, SSA hired another 147 ALJs and over 1,000 support staff for the hearing offices. Until these hires were in place, SSA sent volunteers from its field offices to the hearing offices with the largest backlogs to help assemble paper files. SSA dedicated 5,000 overtime hours per month to the effort (Astrue 2007). SSA plans to hire an additional 226 ALJs in FY 2010 and to maintain a ratio of at least 4.5 support staff members per judge. By the end of FY 2010, ALJs should number about 1,450 (Astrue 2009).
In 2009, SSA opened National Hearing Centers in Albuquerque, Chicago, and Baltimore to supplement its Falls Church, Virginia, center. (In July 2010, SSA plans to open its fifth National Hearing Center, in St. Louis.) At these centers, video conferencing equipment10 has allowed ALJs to hold hearings remotely, with initial efforts focused on the cities where claimants had been waiting the longest. SSA used these centers to issue over 9,000 hearing decisions in FY 2009, and improved average processing times (Astrue 2009). SSA now plans to install video equipment in all hearing rooms to increase hearing capacity. SSA also implemented a Representative Video Project to allow claimant representatives to use their own equipment to participate in hearings from their offices.
SSA has also streamlined the hearing process by reinstituting the Attorney Adjudicator program, which authorizes its most experienced attorneys, when appropriate, to decide on the record in favor of claimants without a hearing. In FY 2009, Attorney Adjudicators issued over 36,000 favorable decisions. SSA is testing a new, more sophisticated screening tool to identify even more cases appropriate for senior attorney review (Astrue 2009).
The agency also instituted special Federal Quality Reviewer screening units and a Medical Expert Screening process to help identify cases that can be allowed without a hearing. In addition, SSA identified cases that were likely to be allowed and electronically transferred them back to the DDSs for further review; the DDSs allowed nearly 15,000 of these claims in FY 2009, eliminating the need for a hearing (Astrue 2009).
On September 20, 2009, Commissioner Astrue announced that for the first time since 1999, the agency had ended the year with fewer disability hearings pending (722,822) than in the prior year (760,813). The agency plans to open 14 new hearing offices and 4 satellite offices by the end of 2010 (SSA 2009j). With continued sufficient funding, SSA aims to eliminate the hearings backlog by 2013 (Astrue 2009).
The Appeals Council has also experienced increased workloads, with an increase of 16 percent in FY 2009 over FY 2008, and an expected additional increase of 12 percent in FY 2010. To deal with pending case increases, SSA has hired 16 new administrative appeals judges, 45 new appeals officers, and almost 200 new paralegals and attorney advisers. Training courses were revamped to shorten the learning curve (Astrue 2009).
SSA also improved the processing of initial disability claims. On September 5, 2007, SSA announced issuance of a final regulation to extend Quick Disability Determination to all state DDSs. A gradual nationwide rollout of the Quick Disability Determination process was completed in February 2008 (SSA 2007a; SSA 2008c). Also in 2008, SSA implemented the Compassionate Allowances initiative to quickly identify diseases and other medical conditions that clearly qualify for disability benefits based on minimal objective medical evidence. The initiative was launched on October 27 with 50 conditions listed (25 cancers and 25 rare diseases) (SSA 2008b). Other diseases and conditions were to be considered for future addition to the list of Compassionate Allowances. On February 11, 2010, SSA announced the addition of 38 conditions (including early-onset Alzheimer's disease) to the list, with the consideration of other conditions to continue (SSA 2010b). On January 28, 2009, SSA announced that improvements to the agency's computer modeling system had increased the number of disability claimants receiving expedited approvals to about 4 percent of all disability cases—numbering about 100,000 to 125,000 per year. This effort helped SSA cope with the increase of about 250,000 cases resulting from the economic downturn (SSA 2009i).
SSA also accelerated the update of its medical listings, which are key factors in determining whether an individual qualifies for disability benefits. By the mid-2000s, many of SSA's listings did not accurately reflect advances in the diagnosis and treatment of certain disorders. The Department of Health and Human Services agreed to join SSA on a task force to update the listings. On October 19, 2007, SSA published its revised medical listings for disorders of the digestive system in the Federal Register, the first update to the listings for these types of disorders in more than 20 years. The new rules became effective on December 18, 2007 (SSA n.d. b; Astrue 2007). SSA hopes to update all of its existing listings by the end of FY 2010, and has developed a schedule to ensure all listings are updated as needed in the future (SSA 2009e, 15).
SSA is also developing a new occupational information system to replace the Dictionary of Occupational Titles, created by DOL. SSA has relied on the dictionary to determine whether claimants can do their usual work, or any other work in the U.S. economy. However, the dictionary was last updated in 1991. In 2008, SSA awarded contracts to help evaluate and update occupational information, and established an Occupational Information Development Advisory Panel for advice on creating an occupational information system tailored to its disability policy (SSA 2009e, 15).
The systems for controlling and processing disability claims in DDSs are also due for replacement. Because they are state agencies, each DDS has developed or contracted for the specialized software used in claims processing. In the 1990s, SSA attempted to develop standardized software that could be used in all DDSs, but most states resisted; only a few locations adopted the Modernized Integrated Disability Adjudicative System (MIDAS) that SSA developed for their use. SSA is trying again to develop a common disability case processing system to replace the legacy DDS systems, and hopes to have a state-of-the-art beta system ready for testing in 2011. This software will enhance SSA's ability to move to electronic medical records (Astrue 2009).
SSA's prospects for reducing its disability workloads deteriorated when the nation entered an economic recession in 2008. Claims volumes increased dramatically. Struck by declining revenues, several states began furloughing employees. Some of these states included state DDS employees in the furloughs even though SSA pays their salaries and all DDS operating costs. Commissioner Astrue urged the states to exempt DDS employees and even enlisted Vice President Joe Biden to echo his plea, but some states continued the furloughs nevertheless (SSA 2009c).
Assisting with the Medicare Prescription Drug Program
Although CMS now administers the Medicare program, SSA continues to provide assistance. For instance, SSA continues to determine individuals' eligibility for Medicare HI and enrolls individuals for Medicare SMI. In addition, SSA assigns the Medicare account number and deducts SMI premiums from OASDI benefits. Since 1998, SSA has also assisted with informing eligible Medicare beneficiaries about the Qualified Medicare Beneficiary (QMB) provision, which pays Medicare premiums for beneficiaries with limited income and resources (SSA n.d. b).
In 2003, SSA assumed another Medicare-related responsibility when the Medicare Prescription Drug, Improvement, and Modernization Act, more commonly known as the Medicare Modernization Act, was enacted. The act created Medicare Part D, a prescription drug program to take effect January 1, 2006. Initial enrollment for Part D ran from November 15, 2005, through May 15, 2006. SSA was tasked with deducting Part D premiums from Social Security payments and administering the low-income subsidy (LIS) program. The LIS or "extra help" program provided for the federal government to cover all or part of the premium, deductible, and copayment costs for eligible Medicare beneficiaries with limited income and resources. Medicare beneficiaries with Medicaid coverage were deemed entitled to the subsidy.
Once again, the legislation provided little time to prepare for implementation. In this case, timely implementation was complicated by dependence on another agency, CMS, to make policy decisions and publish regulations. An entirely new software application was needed to take and process LIS applications. SSA developed not only an online application, but also a scannable paper application. In collaboration with CMS, SSA assembled focus groups of Medicare beneficiaries and conducted special cognitive tests to assess how well potential applicants understood the application. Design engineers reviewed the application layout. In addition, SSA discussed draft versions of the application with national and local advocacy groups and state Medicaid directors (Disman 2006). SSA hired a contractor to test the scannable version on 2,050 potentially eligible individuals to ensure that it was easy for applicants to use. SSA added new fields to the application after 1 year of use to improve the accuracy of the information (Disman 2007).
With no reliable method for identifying those eligible for the LIS (Government Accountability Office 2007, 7), SSA undertook a massive effort to get the word out to all potential applicants. Outreach efforts began in May 2005. SSA mailed a scannable "Application for Help with Medicare Prescription Drug Plan Costs" to almost 19 million potentially eligible Medicare beneficiaries on a staggered basis between May 27 and August 16, 2005. SSA then hired a contractor to make personal follow-up calls between August 18 and November 5, 2005, to almost 12 million potential applicants who did not respond to the mailing. The contractor found phone numbers for about 9 million of these individuals. Applications were resent to 800,000 of them, and 400,000 of them requested assistance and were referred to the agency. SSA sent follow-up letters in the 5 million instances the contractor could not reach the beneficiary after three attempts (McMahon 2006). In a separate exercise, SSA identified about 1.5 million disability beneficiaries who received a subsidy application mailer but did not file. SSA mailed a special follow-up notice to all of these beneficiaries (Disman 2007).
SSA announced its new Internet application for LIS on June 29, 2005, and began taking applications in July (SSA 2005d). The application received one of the highest scores ever given to a public or private sector organization by the University of Michigan's American Customer Satisfaction Index (Disman 2006). As of September, 1,000 people per day were applying over the Internet. By then, SSA's partners had held over 40,000 Medicare outreach events (SSA 2005b). By May 2006, the number of outreach events was up to 72,000. SSA had received applications from more than 4.9 million beneficiaries, of which almost 850,000 were unnecessary (duplicates or applicant already deemed eligible), and had made determinations on 3.9 million applications, finding 1.7 million eligible. SSA held targeted application-taking events in field offices, mailing personal invitations to beneficiaries who had been identified as potentially eligible but had not yet applied for the subsidy (Disman 2006).
By FY 2007, about 22 percent of new applications were internet filings (Disman 2007). Alternatively, individuals could call SSA's 800 number to immediately file an application (McMahon 2006). SSA provided extensive training to its teleservice representatives in answering subsidy-related questions. Callers who wished to apply by phone were referred directly to specialized claims-taking employees (Disman 2006).
The outreach activities continued. SSA recontacted anyone who requested that premiums be withheld from Social Security benefits but had failed to return an LIS application. SSA also mentioned LIS in other outgoing notices. In addition, SSA asked tax preparers who deal with Earned Income Tax Credit filers to screen for LIS (McMahon 2006). SSA worked with states that had their own pharmaceutical programs, state health insurance programs, Area Agencies on Aging, local housing authorities, community health clinics, prescription drug plans, and others to identify people with limited income and resources (Disman 2006).
SSA also targeted mailings to beneficiaries with representative payees, beneficiaries who spoke Spanish, Asian-American and African-American households, and beneficiaries aged 79 or older who lived in zip codes with a high percentage of low-income households. SSA mailed 2.5 million subsidy applications to these individuals between June and August 2006. In September 2006, SSA mailed more than 300,000 applications with CMS notices to Medicare beneficiaries who had lost their deemed-eligible status for the subsidy. The agency began to include subsidy applications with the notices sent each month to approximately 125,000 Social Security beneficiaries when they first become eligible for Medicare. In addition, SSA conducted a special "Mother's Day" initiative to reach out to caregivers in 2007 (Disman 2007).
By March 2007, about 6.2 million individuals had applied for LIS, and SSA had approved approximately 2.2 million applications (Government Accountability Office 2007, 12–13). As of May 2007, SSA was receiving about 30,000 pplications for the LIS every week (Disman 2007).
Surviving Disasters
With over 1,400 locations, SSA offices are occasionally in the path of disasters affecting both the offices themselves and the populations they serve. Although SSA has had disaster procedures in place since early days, coping with the impact can be traumatic.
Given the poor condition of many of SSA's earliest locations, fires were an ever-present threat. Some of the SS-5 Application for Account Number data from the late 1930s are missing because some offices burned before the forms could be mailed to Baltimore. Once SSA began taking claims for benefits, a loss of field office records had more drastic consequences. An account of a fire destroying a field office in the Marion Hotel Building in Marion, Indiana, on the evening of January 31, 1956, states:
Aside from the money required to replace the burned equipment, which will jar DFO's [Division of Field Operations] tight budget somewhat, the major cost of the fire is the loss of 185 pending claims, 7 requests for assistance, 20 recomputation applications, 85 disability freeze applications, and 100 SS-5 applications on which account number cards had been issued. The figures were arrived at by reviewing the regional office copy of the previous week's report and using staff memory. None of the loss is irreparable but a heavy job of redevelopment faces the Marion staff (SSA 1956, 2).
The office was operating in another location in just 36 hours.
Floods have also caused problems. On June 23, 1972, the Wilkes-Barre DOC, which had just assumed responsibility for card punching and keying operations for the central issuance of SSNs, was closed by flood waters caused by Hurricane Agnes. The facility was back in full operation by the end of July (SSA 1972, 74). In June 1976, flooding hit the Wilkes-Barre facility again, putting it out of operation for 2 weeks. As a result, SSA opened another DOC in Salinas to provide backup in case of another disaster (SSA 1976, 7).
In early April 1974, tornadoes ripped through 10 midwestern and southern states, claiming more than 300 lives and causing nearly $1 billion in property damage. One structural casualty was the Nashville DDS office. A tornado tore the roof off of the building, scattering the documents from disability folders and exposing the remaining folders to water damage. SSA employees had to contact thousands of disability applicants to reconstruct their folders (SSA 1973b, 5).
Even microbes have brought SSA facilities low. In September 1991, an individual who worked at the Western PSC in Richmond, California, for a firm under contract to SSA died of Legionnaire's disease. Concerned about employee health, SSA temporarily closed the PSC and tested the building, which was found to be contaminated with Legionnella bacteria. Employees were screened for the bacteria and agency operations were relocated while the facility was decontaminated. The building reopened and employees returned in December 1991 (SSA 1992a, 30).
SSA has not been spared the workings of terrorists. On April 19, 1995, Timothy McVeigh exploded a bomb at the Alfred P. Murrah Federal Building in Oklahoma City. An SSA field office was located on the first floor of the building. Sixteen SSA employees were among the 168 people who lost their lives (Harmon and others 2000).
SSA was also affected by the September 11, 2001, terrorist attacks on the World Trade Center in New York City. The New York regional office, three field offices, and a hearing office were all near the World Trade Center and were closed in the aftermath of the attack. The regional office relocated, and the field office employees and hearing workloads were distributed to other locations until they could be reopened. The New York DDS was also affected. The employees were temporarily relocated, and the 15,000 case folders pending at the time of the attack were removed, cleaned, tested, and certified to be contaminant-free (SSA 2001c).
When disaster strikes a community, the agency's concerns are broader than just setting up shop in a new location. After the 9/11 attack, SSA invoked special emergency procedures to get immediate help to the families of those killed in the World Trade Center, the Pentagon, and the Flight 93 plane crash in Shanksville, Pennsylvania. These procedures were designed to take and pay claims as quickly as possible and included allowing the payment of survivors' claims using airline manifests or employer records rather than waiting for a death certificate. SSA immediately launched a full-scale outreach effort to locate families of the victims. SSA posted a special Web page with information on applying for benefits and links to various other sites. The agency arranged for public information spots on every major network affiliate in New York City, as well as on independent and Spanish language stations. It distributed press releases and fact sheets to national and local media outlets and advocacy organizations, among others. SSA also worked with the uniformed services and with the 58 employers who lost employees in the World Trade Center for follow-up. In addition, SSA reached out to 60 consulates to ensure that any foreign survivors who might be eligible for benefits were contacted (SSA 2002a, 1–2).
SSA stationed hundreds of employees at the Pier 94 Family Assistance Center and in other crisis centers throughout New York, at the Liberty State Park Family Assistance Center in New Jersey, and at the Pentagon Family Assistance Center. SSA staff was available to serve the families of the victims of the Flight 93 crash in Shanksville and in other locations. Those families could visit any of these sites, any field office, or call the SSA 800 number to file an immediate claim (SSA 2002a, 2–3). As of 2 years later, SSA had processed 5,629 benefit claims from 2,281 families, and was paying ongoing benefits to 3,228 survivors and 498 individuals disabled during the attacks (Szymendera 2005, 5).
A more recent natural disaster, Hurricane Katrina on August 29, 2005, also tested SSA's emergency response capabilities. In Louisiana, more than 400,000 OASDI beneficiaries and 91,000 SSI recipients resided in the counties affected by Hurricane Katrina; in Mississippi, about 127,000 OASDI beneficiaries and 22,000 SSI recipients lived in the areas impacted; and in Alabama, almost 125,000 OASDI beneficiaries and 21,000 SSI recipients were affected (SSA 2005c). Seventy-three SSA field offices and a number of DDSs closed temporarily because of the hurricane. Some were not damaged, but others were flooded or even submerged. By September 8, all but 11 field offices had reopened, many in temporary space. SSA transported six portable buildings to south Louisiana for use as field offices. All affected DDSs were reopened by September 6, 2005 (SSA 2005a). The Electronic Disability System enabled SSA to immediately transfer the 1,500 cases that had been stored electronically in the New Orleans DDS. For the remaining 3,500 cases, SSA packed the folders in 400 boxes and carted them down 6 flights of stairs guided by flashlight (Barnhart 2006).
SSA opened temporary offices at evacuation centers such as the Houston Astrodome, the Baton Rouge River Center, the Albuquerque Convention Center, the Lubbock Reese Center, and the El Paso and Dallas Convention Centers. In addition, SSA had at least one employee staffing each of more than 50 Federal Emergency Management Agency sites, working 12-hour days and weekends in some cases. Many of the local offices that were still able to operate extended their service hours and remained open throughout the Labor Day weekend. The Dallas Regional Office opened a temporary Field Office Support Unit in its training center to assist with claims. SSA detailed 139 employees from other regions to assist the affected field offices and DDSs assigned extra employees to answer calls to the 800 number. SSA placed special flags on all Katrina-related initial claims to ensure expedited handling and instituted special procedures for establishing identity for beneficiaries without traditional forms of photo identification (SSA 2005a).
In areas where mail service was suspended, SSA and the U.S. Postal Service established Temporary Mail Delivery Stations where beneficiaries could pick up their checks. As of September 8, 2005, 15,000 checks had been delivered at the temporary stations. To ensure that beneficiaries continued to receive their OASDI and SSI payments, SSA also invoked an immediate payment procedure that permitted on-the-spot disbursements to those who could not access their benefit checks. As of September 9, SSA had issued more than 30,000 immediate payments (SSA 2005c). When Louisiana sites began to run short of the Third Party Disposition forms used for the immediate payments and FedEx was unable to assure delivery, SSA set up a relay chain for passing along additional forms from one field office to the next until finally the Lafayette, Louisiana, office delivered them to Baton Rouge (SSA 2005a).
Always cognizant of the possibility of unexpected disaster, SSA has a robust continuance-of-operations plan, and regularly tests its recovery procedures. In January 2009, SSA opened a second data support center in North Carolina that can be used not only for processing its high volume of transactions but also for disaster recovery should Baltimore National Computer Center operations be disrupted. In addition, Congress appropriated $500 million to build and partially equip a new, modern data center to replace the now-outmoded Baltimore facility (Astrue 2009).
Today
New challenges will always arise to replace old ones. Beginning in 2008, the recession caused SSA workloads to spike once again. Even with 800-number and Internet options for public contact, field offices averaged 866,000 visitors per week in 2009. In FY 2009, SSA processed over 175,000 more initial disability claims than anticipated, while some states began to furlough employees in the state-administered DDSs—even though SSA pays the employees' salaries (Astrue 2009). SSA's productivity increased nearly 30 percent from 2005 to 2009 (SSA 2009d, 79), yet employees are struggling to keep up with the work. In 2008, 50 percent of callers to SSA field offices received a busy signal, and 8 percent of those visiting a field office without an appointment—about 3 million visitors—had to wait more than an hour to be seen by staff. Although field offices continue to process initial claims timely, they have been forced to defer processing millions of postentitlement events such as adjusting payments and correcting earnings postings. This is not only unacceptable service, it is also demoralizing to SSA's employees, who care deeply about the level of service they provide (McMahon 2008).
Some help has arrived. In FY 2009, Congress provided SSA with Recovery Act funds to assist with the rising workloads and hearings backlog. SSA's administrative budget also increased. In FY 2009, SSA hired approximately 8,600 new employees, its biggest hiring effort since the SSI program launch 35 years earlier. SSA budgeted for 2,600 more DDS employees, as well. Funds were also used to purchase additional computers, for video conferencing equipment for hearings, and to contract with additional medical providers and networks (Astrue 2009).
Nevertheless, claims workloads are still growing faster than SSA can process them. In FY 2010, SSA expects to receive 1.2 million more claims than in FY 2008. Over 3.3 million disability claims alone are expected, a 27 percent increase over FY 2008. As the workloads grow, 50 percent of SSA's workforce, including 66 percent of its supervisors, will be eligible to retire by the end of 2018 (SSA 2009e, 18).
To handle these additional cases, SSA is experimenting with video service to enable staff in less busy offices to assist offices that may be overwhelmed with visitors, or to contact persons who live in remote areas (Astrue 2009). Also, SSA plans to establish centralized units, similar to the National Hearing Centers, to assist the DDSs. These new units, called Extended Service Teams, will be located in states that have a history of high quality and productivity and that have the capacity to hire and train additional staff. The teams will be used to quickly take cases from the highest-volume states. In FY 2010, SSA plans to place 280 new employees in Virginia, Arkansas, Oklahoma, and Mississippi. SSA is also expanding case processing capacity in its 10 regional disability units and the Federal Disability Center in Baltimore. SSA is also once again deferring some CDRs so that the DDSs can concentrate on initial claims (Astrue 2009).
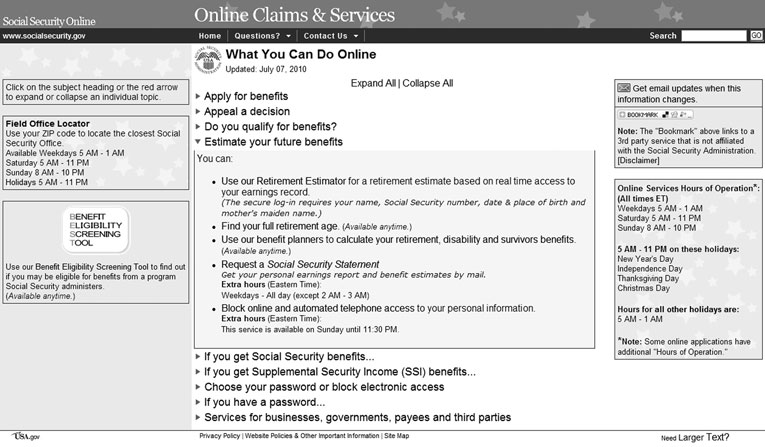
SSA Web site, http://www.socialsecurity.gov/onlineservices/.
SSA also hopes that by providing Internet tools, the public will increasingly be able to help themselves. In December 2008, SSA launched the new version of its online Internet claims process, called iClaim. A marketing campaign starring actress Patty Duke accompanied the launch. The online share of retirement applications increased from 26 percent to 35 percent in less than 1 month, and the online share of disability claims increased from 14 percent to 21 percent. SSA hopes to increase these percentages in 2010 to 38 percent and 25 percent, respectively (Astrue 2009).
In July 2008, SSA updated its Internet-based application for estimating retirement benefits. This version is tied into SSA's earnings records, eliminating the need for the user to manually enter years of earnings information. The Retirement Estimator is interactive, allowing a person to compare different retirement options (SSA 2008a). In November 2008, the American Customer Satisfaction Index for federal Web sites ranked the new online Retirement Estimator as the best in government (SSA 2008d). In its first year of operation, the Retirement Estimator provided over 4 million estimates. In November 2009, the Retirement Estimator was improved to provide benefit estimates for people who had enrolled in Medicare but not yet for Social Security benefits—a cohort numbering about a half million each year. In 2010, SSA will release a Spanish language version (SSA 2009g).
Individuals can use the Internet to find information about SSA-administered programs, locate a Social Security office, or request a Social Security Statement. With a password, beneficiaries may check their benefits, change an address, and start or change direct deposit payments. Beneficiaries may also change their address without a password. In addition, beneficiaries can request a Medicare replacement card, a benefit verification letter, and a replacement Form 1099 using knowledge-based authentication. Businesses can use the Internet to file Form W-2s for employees or verify SSNs.
Other technology investment plans for 2010 and beyond involve "Disability Direct" to automate the processing of online disability claims, signature proxy alternatives to pen-and-ink or "wet" signatures, voice over Internet protocol telephone networks for the field offices, "click to talk" capability to connect Internet visitors with a teleservice representative, and self-help computers in field office reception areas (SSA 2009e, 17).
Conclusion
Although SSA has changed in many ways over the years, the root causes of its administrative challenges have remained much the same throughout its existence.
A 1993 GAO report stated:
SSA's ability to carry out its mission is affected by various external factors over which it has little or no control. These include (1) frequent legislative changes that affect program administration; (2) conflicting views between and within the administration and the Congress on how SSA should operate; (3) the need to comply with decisions or requirements of central management agencies, such as the Office of Management and Budget (OMB); and (4) a high degree of dependence on others, such as states and employers, to provide accurate and timely data needed for program administration (GAO 1993, 13).
SSA has been blessed with a workforce that believes in the agency's mission and sincerely cares about program beneficiaries. These dedicated employees have helped SSA become one of the best agencies in the federal government. In April 2007 and again in May 2009, the Partnership for Public Service and American University's Institute for the Study of Public Policy Implementation ranked SSA as one of the top ten "best places to work in the federal government." The rating was based on the results of the Office of Personnel Management's Federal Human Capital Survey, a governmentwide assessment of federal employees' job satisfaction and perceptions of their agency's human capital efforts (SSA 2007c; SSA 2009h).
SSA has overcome many difficult challenges in its 75-year history, and will no doubt weather the current recession as well. SSA has a history of rising to its challenges and evolving to meet society's changing needs. Some may doubt that Social Security will be there for them in the future, but such an absence is highly unlikely. SSA is a survivor.
Notes
1 In May 2009 SSA estimated that in fiscal year 2010, it would process an additional 20,000 retirement claims and 200,000 initial disability claims over the fiscal year 2009 levels (SSA 2009e, 11).
2 Predecessor of the Works Progress Administration.
3 A trading zone is the area beyond an urban area whose residents regularly trade with merchants within the urban area.
4 The disability freeze only excluded the years a person was disabled from the computation of benefits; it did not provide for monthly payments.
5 Material participation means participation on a regular or substantial basis in the production of farm commodities.
6 The medical listing of impairments describes examples of common impairments that SSA considers severe enough to keep an adult from doing any gainful activity.
7 A CDR is a review of a beneficiary's current medical condition to see if it is still disabling.
8 An essential person was defined as someone who had continuously lived in the qualified individual's home since December 1973, was not eligible for state assistance in December 1973, and had never been eligible for SSI payments as an eligible individual or as an eligible spouse. In addition, state records had to show that, under a state plan in effect for June 1973, the state took that person's needs into account in determining the qualified individual's need for state assistance for December 1973.
9 Individuals who had not worked sufficiently to qualify for HI could purchase coverage if they were willing to pay the monthly premium. Some states paid the premiums for low-income individuals.
10 SSA began testing video teleconferencing for hearings with claimants, representatives, or expert witnesses at remote locations in the late 1990s. By 2004, approximately 160 hearings rooms were equipped, and about 8,000 hearings used video teleconferencing (Apfel 2000).
References
[Advisory Council] Advisory Council on Social Security. 1965. Report of the Advisory Council on Social Security: The status of the Social Security program and recommendations for its improvement. Social Security Bulletin 28(3): 3–41. Available at http://www.socialsecurity.gov/policy/docs/ssb/v28n3/v28n3p3.pdf.
Altmeyer, Arthur J. 1966. The formative years of Social Security. Madison, WI: The University of Wisconsin Press.
Apfel, Kenneth S. 2000. Testimony before the House Committee on Ways and Means, Subcommittee on Social Security. Social Security's readiness for the impending wave of baby boomer beneficiaries (March 16). 106th Cong., 2nd sess. Committee on Ways and Means Serial No. 106-44. Available at http://www.socialsecurity.gov/legislation/testimony_031600.html.
Astrue, Michael J. 2007. Testimony before the Senate Committee on Finance. Funding Social Security's administrative costs: Will the budget meet the mission? (May 23). 110th Cong., 1st sess. Senate Hearing No. 110-715. Available at http://www.socialsecurity.gov/legislation/testimony_052307.htm.
———. 2009. Testimony before the House Committee on Ways and Means, Subcommittee on Social Security. Clearing the disability claims backlogs: The Social Security Administration's progress and new challenges arising from the recession (November 19). 111th Cong., 1st sess. Available at http://www.socialsecurity.gov/legislation/testimony_111909.htm.
Ball, Robert M. 1965. A report on the implementation of the 1965 amendments to the Social Security Act. Available at http://www.socialsecurity.gov/history/medreport.html.
Barnhart, Jo Anne. 2006. Testimony before the Senate Committee on Finance. Administrative Challenges Facing the Social Security Administration (March 14). 109th Cong., 2nd sess. Senate Hearing No. 109-733. Available at http://www.socialsecurity.gov/legislation/testimony_031406.html.
[Board of Trustees] Board of Trustees of the Federal Old-Age and Survivors Insurance and Federal Disability Insurance Trust Funds. 2009. The 2009 annual report of the Board of Trustees of the Federal Old-Age and Survivors Insurance and Federal Disability Insurance Trust Funds. Washington, DC: Government Printing Office. Available at http://www.socialsecurity.gov/OACT/TR/2009/.
Bowers, Ronald P., and Robert V. Korycki. 1970. Planning for the future of the Bureau of Retirement and Survivors Insurance. Baltimore, MD: SSA, Bureau of Retirement and Survivors Insurance.
Casey, Jack. 1977. The use of advanced technology in the administration of the Social Security system in the United States of America. Baltimore, MD: SSA, Office of Advanced Systems.
Christgau, Victor. 1955. Old-age and Survivors Insurance after twenty years. Social Security Bulletin 18(8): 12–17.
Cohen, Wilbur J., and Robert J. Myers. 1950. Social Security Act Amendments of 1950: A summary and legislative history. Social Security Bulletin 13(10): 3–14. Available at http://www.socialsecurity.gov/history/1950amend.html.
Corson, John J. 1938. Administering Old-Age Insurance. Social Security Bulletin 1(5): 3–6. Available at http://www.socialsecurity.gov/history/corson538.html.
Davis, John A. 1950. Regional organization of the Social Security Administration: A case study. New York, NY: Columbia University Press.
Department of Health, Education, and Welfare. 1966. Annual Report, U. S. Department of Health, Education, and Welfare. Washington, DC: Government Printing Office.
Derthick, Martha. 1990. Agency under stress: The Social Security Administration in American government. Washington, DC: Brookings Institution Press.
DeWitt, Larry. 1997. The Civilian War Benefits Program: SSA's first disability program. Social Security Bulletin 60(2): 68–76. Available at http://www.socialsecurity.gov/policy/docs/ssb/v60n2/v60n2p68.pdf.
Disman, Beatrice. 2006. Testimony before the House Committee on Ways and Means, Subcommittee on Health. Medicare drug benefit implementation (May 3). 109th Cong., 2nd sess. Available at http://www.socialsecurity.gov/legislation/testimony_050306.html.
———. 2007. Testimony before the Senate Committee on Finance. Medicare prescription drug benefit: Review and oversight (May 8). 110th Cong., 1st sess. Senate Hearing No. 110-574. Available at http://www.socialsecurity.gov/legislation/testimony_050807.htm.
Fay, Joseph L., and Max J. Wasserman. 1938. Accounting operations of the Bureau of Old-Age Insurance. Social Security Bulletin 1(6): 24–28. Available at http://socialsecurity.gov/history/fay638.html.
Federal Security Agency. 1948. Annual report of the Federal Security Agency for the fiscal year 1947: Section one, Social Security Administration. Washington DC: Government Printing Office.
———. 1950. Annual report of the Federal Security Agency 1950: Social Security Administration. Washington, DC: Government Printing Office.
FSA. See Federal Security Agency.
Futterman, Jack S. 1960. Some techniques of management improvements in the administration of the Social Security in the United States. Paper presented to the Regional Committee on Organization and Methods of the Inter-American Committee on Social Security of the International Social Security Association.
GAO. See General Accounting Office.
General Accounting Office. 1989. Social Security: Status and evaluation of agency management improvement initiatives. GAO/HRD-89-42. Washington, DC: Government Printing Office.
———. 1993. Social Security: Sustained effort needed to improve management and prepare for the future. GAO/HRD-94-22. Washington, DC: Government Printing Office.
———. 1997. Social Security Administration: More cost-effective approaches exist to further improve 800-number service. GAO/HEHS-97-79. Washington, DC: Government Printing Office.
Gerry, Martin H. 2006. Submission for the record to the House Committee on Ways and Means, Subcommittee on Human Resources. Use of technology to improve public benefit programs (April 5). 109th Cong., 2nd sess. Committee on Ways and Means Serial No. 109-69. Available at http://www.socialsecurity.gov/legislation/testimony_040506.html.
Gluck, M.G., and Reno, V., eds. 2001. Reflections on implementing Medicare. Washington, DC: National Academy of Social Insurance. Available at http://www.nasi.org/usr_doc/med_report_reflections.pdf.
Government Accountability Office. 2007. Medicare Part D Low-Income Subsidy: Progress made in approving applications, but ability to identify remaining individuals is limited. Testimony before the Senate Committee on Finance. GAO-07-858T. Washington, DC: Government Printing Office.
Harmon, Wayne, Jim Demer, Melvin Files, Maryanne Lysett, Lydia Marshall, and Bill Shie. 2000. A history of the Social Security Administration during the Clinton Administration 1993–2001. Available at http://www.socialsecurity.gov/history/ssa/ssa2000history.html.
Hensley, Rich. 1994. From the editor. OASIS 40(1): 2. Available at http://www.socialsecurity.gov/history/oasis/january1994.pdf.
HEW. See Department of Health, Education, and Welfare.
House Ways and Means Committee. See U.S. Congress, House Committee on Ways and Means.
Ladd, Boyd, Thomas D. Scriggins, Conway J. Christianson, and John H. Moss. 1961. Operation research for OASDI service in a changing future. Baltimore, MD: The Johns Hopkins University Press.
Long, Wayne S. 1993. Social Security numbers issued: A 20-year review. Social Security Bulletin 56(1): 83–86. Available at http://www.socialsecurity.gov/policy/docs/ssb/v56n1/v56n1p83.pdf.
Lowrey, Perrin. 1955. Everybody's a farm expert. OASIS 1(1): 5, 13.
Maldonado, Joe P. 1978. Assessment of SSA service to the public. SSA internal document.
McKenna, Hugh F. 1976. Report of Social Security Administration's efforts to improve productivity. SSA internal document.
McKinley, Charles, and Robert W. Frase. 1970. Launching Social Security: A capture-and-record account, 1935–1937. Madison, WI: The University of Wisconsin Press.
McMahon, Linda S. 2006. Testimony before the Senate Special Committee on Aging. Meeting the challenges of Medicare drug benefit implementation (February 2). 109th Cong., 2nd sess. Special Committee on Aging Serial No. 109-17. Available at http://www.socialsecurity.gov/legislation/testimony_020306.html.
———. 2008. Testimony before the Senate Committee on Finance. Social Security Field Offices (May 8). 110th Cong., 2nd sess. Available at http://www.socialsecurity.gov/legislation/testimony_050808.htm.
National Research Council. 1990. A report prepared by the Committee on Review of the SSA's System Modernization Plan (SMP) and Agency Strategic Plan (ASP). Washington, DC: National Academy Press.
Office of Technology Assessment. 1986. The Social Security Administration and information technology—special report, OTA-CIT-311. Washington, DC: Government Printing Office. Available at http://www.socialsecurity.gov/history/pdf/ota86.pdf.
Olcott, Mace. 1981. On the homefront: SSA, like everyone else, contributed to the war effort in World War II. OASIS 27(11): 14–17. Available at http://www.socialsecurity.gov/history/oasis/december1981.pdf.
OTA. See Office of Technology Assessment.
Pogge, Oscar C. 1952. After fifteen years: A report on Old-Age and Survivors Insurance. Social Security Bulletin 15(1): 3–14.
Rust, David A. 2008. Testimony before the Senate Committee on Homeland Security and Governmental Affairs, Subcommittee on Federal Financial Management, Government Information, and International Security. Eliminating agency payment errors (January 31). 110th Cong., 2nd sess. Senate Hearing No. 110-501. Available at http://www.socialsecurity.gov/legislation/testimony_013108.htm.
Simmons, Carole. 1977. The way we were: A look back at beauty contests, streetcars, and the PBX board. OASIS 23(1): 11–13. Available at http://www.socialsecurity.gov/history/oasis/january1977.pdf.
Social Security Administration. 1950. OASIS News: Ten years ago—January 1950. Available at http://www.socialsecurity.gov/history/oasis/oasisnews1.html.
———. 1952a. Account number problems. Baltimore, MD: SSA Division of Field Operations, Division of Accounting Operations.
———. 1952b. The Bureau: A profile. OASIS News 12(1). Available at http://www.socialsecurity.gov/history/oasis/oasisnews3.html.
———. 1955a. The field—then and now. OASIS 1(8): 10–13, 21–22, 30.
———. 1955b. Philadelphia (a.o.) story. OASIS 1(2): 4–5, 14.
———. 1955c. Standing room only. OASIS 1(2): 2.
———. 1956. The impossible takes a day and a half. OASIS 2(3): 2, 12.
———. 1960a. The Bureau: 1935–1960. OASIS 6(8): 31–34. Available at http://www.socialsecurity.gov/history/oasis/august1960.pdf.
———. 1960b. District offices. OASIS 6(8): 26–29. Available at http://www.socialsecurity.gov/history/oasis/august1960.pdf.
———. 1960c. Electronic data processing in the Division of Accounting Operations. Baltimore, MD: SSA Bureau of Old Age and Survivors Insurance.
———. 1964a. John Corson recalls…former director of BOASI recounts. OASIS 10(5): 4–5. Available at http://www.socialsecurity.gov/history/oasis/may1964.pdf.
———. 1964b. Social Security U.S.A.—the program and its administration. Available at http://www.socialsecurity.gov/history/ssa/usa1964.html.
———. 1965. The field: 1935–65. OASIS 11(8): 30–34. Available at http://www.socialsecurity.gov/history/oasis/august1965.pdf.
———. 1966. Documentation and decision making in Social Security claims. Baltimore, MD: SSA, Bureau of Retirement and Survivors Insurance.
———. 1967a. Oral history collections: John J. Corson. Interview by Abe Bortz. Available at http://www.socialsecurity.gov/history/corsonoral.html.
———. 1967b. SSA annual report, fiscal year 1967. Washington, DC: Government Printing Office.
———. 1969. SSA annual work plan report, fiscal year 1969. SSA internal document.
———. 1970. Annual report of the Social Security Administration fiscal year 1970. Washington, DC: Government Printing Office.
———. 1971. SSA annual report: Program administration and organizational activities for fiscal year 1971. Washington, DC: Government Printing Office.
———. 1972. The administration of Social Security programs—1972: The year in review. Washington, DC: Government Printing Office.
———. 1973a. Bureau of Data Processing operations. Baltimore, MD: SSA, Bureau of Data Processing.
———. 1973b. The year in review: The administration of Social Security programs—1973. Washington, DC: Government Printing Office.
———. 1974a. Oral history collections: Milton Freedman. Interview by O.R. Garcia. Available at http://www.socialsecurity.gov/history/miltforal.html.
———. 1974b. The year in review: The administration of Social Security programs—1974. Washington, DC: Government Printing Office.
———. 1975a. Oral history collections: David L. Kopelman. Interview by O.R. Garcia. Available at http://www.socialsecurity.gov/history/davidkoral.html.
———. 1975b. Oral history collections. Elmer C. Lupton. Interview by O.R. Garcia. Available at http://www.socialsecurity.gov/history/luptonoral.html.
———. 1975c. The year in review: The administration of the Social Security programs—1975. Washington, DC: Government Printing Office.
———. 1976. The year in review: The administration of Social Security programs—1976. Washington, DC: Government Printing Office.
———. 1978a. Annual report of the Social Security Administration, fiscal year 1977. Washington, DC: Government Printing Office.
———. 1978b. The year in review: The administration of Social Security programs 1978. Washington, DC: Government Printing Office.
———. 1979. A quarter century of aiding the disabled. OASIS 25(11): 22–26. Available at http://www.socialsecurity.gov/history/oasis/november1979.pdf.
———. 1980a. Annual report of the Social Security Administration, fiscal year 1979. Washington, DC: Government Printing Office.
———. 1980b. The year in review: The administration of Social Security programs—1979. Washington, DC: Government Printing Office.
———. 1982a. Social Security annual report to the Congress for fiscal year 1981. Washington, DC: Government Printing Office.
———. 1982b. Systems Modernization Plan: From survival to state of the art. Baltimore, MD: SSA.
———. 1983. Social Security Administration, 1983 annual report to the Congress. Baltimore, MD: SSA.
———. 1984a. Social Security Administration, 1984 annual report to the Congress. Baltimore, MD: SSA.
———. 1984b. SSA and SSI: The tenth anniversary. OASIS 30(1): 14–19. Available at http://www.socialsecurity.gov/history/oasis/january1984.pdf.
———. 1985a. Social Security Administration, 1985 annual report to the Congress. Baltimore, MD: SSA.
———. 1985b. SSA "pioneers" recall the early days. OASIS 31(7): 12–17. Available at http://www.socialsecurity.gov/history/oasis/julyaugust1985.pdf.
———. 1986. SSA Systems Modernization Plan 1986, field edition. Baltimore, MD: SSA.
———. 1987. Social Security Administration 1987 annual report to the Congress. Baltimore, MD: SSA.
———. 1988. Social Security Administration 1988 annual report to the Congress. Baltimore, MD: SSA.
———. 1990. Social Security Administration 1990 annual report to the Congress. Baltimore, MD: SSA.
———. 1991. Social Security Administration 1991 annual report to the Congress. Baltimore, MD: SSA.
———. 1992a. Social Security Administration 1992 annual report to the Congress. Baltimore, MD: SSA.
———. 1992b. We're in the Smithsonian! Major exhibition includes our card punch operations. OASIS 38(5): 15. Available at http://www.socialsecurity.gov/history/oasis/june1992.pdf.
———. 1994a. SSI marks 20 years: 'The greatest challenge (SSA) has ever had.' OASIS 40(1): 4–5. Available at http://www.socialsecurity.gov/history/oasis/january1994.pdf.
———. 1994b. Twentieth anniversary: How SSA met the challenge. OASIS 40(1): 6–9. Available at http://www.socialsecurity.gov/history/oasis/january1994.pdf.
———. 1995a. A brief history of the Social Security Administration: Issued on the occasion of the Social Security Administration's Independent Agency Ceremony. Baltimore, MD: SSA.
———. 1995b. A look back: Medicare program celebrates 30th anniversary. OASIS 41(6): 31. Available at http://www.socialsecurity.gov/history/oasis/july1995.pdf.
———. 1995c. Oral history collections: Ed Tall. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/tall.html.
———. 1995d. Oral history collections: George Failla. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/failla.html.
———. 1995e. Oral history collections: Huldah Lieberman. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/orals/HLieberman.html.
———. 1995f. Oral history collections: Jacob (Jack) Schmulowitz. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/schmlrv2.html.
———. 1995g. Oral history collections: John Ritter. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/ritter6.html.
———. 1995h. Oral history collections: Renato Anthony DiPentima. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/renny.html.
———. 1996a. Oral history collections: Arthur F. Simermeyer. Interviews by Larry DeWitt. Available at http://www.socialsecurity.gov/history/simermeyer.html.
———. 1996b. Oral history collections: Bob Bynum. Interviews by Larry DeWitt. Available at http://www.socialsecurity.gov/history/orals/bynum.html.
———. 1996c. Oral history collections: Herb Borgen. Interviews by Larry DeWitt. Available at http://www.socialsecurity.gov/history/hboral.html.
———. 1996d. Oral history collections: Lillie Steinhorn. Interview by Bob Krebs. Available at http://www.socialsecurity.gov/history/lsoral.html.
———. 1996e. Oral history collections: Manny Levine. Interview by Larry DeWitt. Available at http://www.socialsecurity.gov/history/ml.html.
———. 1997a. Oral history collections: Jack S. Futterman. Interviews by Larry DeWitt. Available at http://www.socialsecurity.gov/history/futterman.html.
———. 1997b. Statement by Kenneth S. Apfel, Commissioner of Social Security, on SSI Childhood Disability Reviews. SSA News Release (December 17). Available at http://www.socialsecurity.gov/pressoffice/childhood_statement.html/.
———. 2001a. Inspector General Statement on the Social Security Administration's major management challenges. Baltimore, MD: SSA, Office of the Inspector General.
———. 2001b. Oral history collections: Robert Ball. Interviews by Larry DeWitt. Available at http://www.socialsecurity.gov/history/orals/balloralhistory.html.
———. 2001c. Social Security Administration responds to terrorist attacks on America. SSA News Release archives. Available at http://www.socialsecurity.gov/pressoffice/releaseattack.htm.
———. 2002a. OASIS special edition. Available at http://www.socialsecurity.gov/history/oasis/911OASIS.pdf.
———. 2002b. Performance plan, appendix 5. Available at http://www.socialsecurity.gov
———. 2003. Social Security Administration performance and accountability report, fiscal year 2003. Baltimore, MD: SSA.
———. 2005a. Hurricane Katrina actions. SSA internal documents.
———. 2005b. More than three million people apply for Medicare Prescription Drug Help. SSA News Release (September 22). Available at http://www.socialsecurity.gov/pressoffice/pr/MedicareHelp2-pr.htm.
———. 2005c. Social Security responds to Hurricane Katrina: Agency issues more than 30,000 emergency checks to date. SSA News Release (September 9). Available at http://www.socialsecurity.gov/pressoffice/pr/katrina-pr-alt.pdf.
———. 2005d. Social Security website—www.socialsecurity.gov—newest location for people to apply for extra help with their Medicare prescription drug costs. SSA News Release (June 29). Available at http://www.socialsecurity.gov/pressoffice/pr/MedicareHelp-pr.htm.
———. 2007a. Commissioner Astrue extends Social Security's quick disability determination nationwide: Final rule will accelerate benefits to those deemed clearly disabled. SSA News Release (September 5). Available at http://www.socialsecurity.gov/pressoffice/pr/qdd-process-pr.htm.
———. 2007b. Social Security Administration attacks disability backlog. SSA News Release (October 9). Available at http://www.socialsecurity.gov/pressoffice/pr/disability-backlog-pr.htm.
———. 2007c. Social Security rated one of the "best places to work in the federal government." SSA News Release (April 19). Available at http://www.socialsecurity.gov/pressoffice/pr/bestplacetowork-pr.htm.
———. 2008a. Estimate your Social Security retirement benefits online now at www.socialsecurity.gov/estimator. SSA News Release (July 21). Available at http://www.socialsecurity.gov/pressoffice/pr/ret-est-pr-draft.htm.
———. 2008b. Social Security announces nationwide launch of compassionate allowances; process will fast track applications for people with cancers and rare diseases. SSA News Release (October 27). Available at http://www.socialsecurity.gov/pressoffice/pr/compassionate-allowances-1008-pr.htm.
———. 2008c. Social Security continues to make progress expediting backlogged disability cases; limited resources under a continuing resolution could slow momentum in FY 2009. SSA News Release (October 17). Available at http://www.socialsecurity.gov/pressoffice/pr/backlog-progress-pr.html.
———. 2008d. Social Security's new Retirement Estimator rated the federal government's best online service. SSA News Release (November 3). Available at http://www.socialsecurity.gov/pressoffice/pr/ACSIestimator-pr.htm.
———. 2008e. Strategic plan fiscal years 2008–2013. Baltimore, MD: SSA. Available at http://www.socialsecurity.gov/asp/index.htm.
———. 2009a. Annual Statistical Supplement to the Social Security Bulletin, 2008. Washington, DC: Office of Retirement and Disability Policy, Office of Research, Evaluation, and Statistics. Available at http://www.socialsecurity.gov/policy/docs/statcomps/supplement/2008/index.html.
———. 2009b. A brief history of SSA program instructions. SSA internal document. Baltimore, MD: SSA Office of PolicyNet and Program Support (OPPS).
———. 2009c. Commissioner Astrue asks governors to exempt state Disability Determination Service employees from hiring restrictions. SSA News Release (February 3). Available at http://www.socialsecurity.gov/pressoffice/pr/dds-hiring-pr.html.
———. 2009d. Performance and accountability report for fiscal year 2009. Available at http://www.socialsecurity.gov/finance/2009/Full%20FY%202009%20PAR.pdf.
———. 2009e. Social Security Administration justification of estimates for Appropriation Committees, fiscal year 2010. Available at http://www.socialsecurity.gov
———. 2009f. Social Security Administration retirement wave report: Component/regional analysis, fiscal years 2009–2018. Baltimore, MD: SSA Human Capital Planning Staff.
———. 2009g. Social Security announces new enhancements to online Retirement Estimator. SSA News Release (November 13). Available at http://www.socialsecurity.gov/pressoffice/pr/online-retirement-estimator-pr.htm.
———. 2009h. Social Security continues to rank as one of the "best places to work in the federal government." SSA News Release (May 20). Available at http://www.socialsecurity.gov/pressoffice/pr/bestplacetowork2-pr.htm.
———. 2009i. Social Security expands fast-track disability processes; more than 100,000 disabled applicants get quick decisions. SSA News Release (January 28). Available at http://www.socialsecurity.gov/pressoffice/pr/disability-fast-track-pr.html.
———. 2009j. Social Security hearings backlog down for first time in decade; productivity and processing times also improve. SSA News Release (September 30). Available at http://www.socialsecurity.gov/pressoffice/pr/hearings-backlog-pr.htm.
———. 2009k. Social Security to fund $24 million in contracts for electronic medical records. SSA News Release (August 7). Available at http://www.socialsecurity.gov/pressoffice/pr/electronic-med-records-pr.htm.
———. 2009l. Unpublished information. Office of Public Service and Operations Support.
———. 2010a. Health information technology update. SSA Commissioner's Broadcast (February 1). SSA internal document.
———. 2010b. Social Security adds 38 new compassionate allowance conditions; expansion will speed benefits to thousands of Americans with Disabilities. SSA News Release (February 11). Available at http://www.socialsecurity.gov/pressoffice/pr/cal021110-pr.html.
———. No date a. History of SSA during the Johnson Administration 1963–1968. Available at http://www.socialsecurity.gov/history/ssa/lbjhistory.html.
———. No date b. Special collections: Detailed chronology. Available at http://www.socialsecurity.gov/history/chrono.html.
———. No date c. SSA History: Brief graphic organizational history. Available at http://www.socialsecurity.gov/history/orghist.html.
SSA. See Social Security Administration.
Staruch, George. 1978. The way we were: Filing little wooden sticks. OASIS 24(3): 29–30. Available at http://www.socialsecurity.gov/history/oasis/march1978.pdf.
Swift, Roy. 1960. A quarter century of public information. OASIS 6(9): 11–13, 23. Available at http://www.socialsecurity.gov/history/oasis/september1960.pdf.
Szymendera, Scott. 2005. Hurricane Katrina: Activities of the Social Security Administration. Washington, DC: Congressional Research Service. Available at http://www.au.af.mil/au/awc/awcgate/crs/rs22250.pdf.
U.S. Congress, House Committee on Ways and Means. 1973. Annual report of the Social Security Administration for fiscal year 1972: Submitted to the Congress by the Department of Health, Education, and Welfare on March 9, 1973. Washington, DC: Government Printing Office.
———. 1974. Annual report of the Social Security Administration for fiscal year 1973: Submitted to the Congress by the Department of Health, Education, and Welfare on February 26, 1974. Washington, DC: Government Printing Office.
———. 1975. Annual report of the Social Security Administration for fiscal year 1974: Submitted to the Congress by the Department of Health, Education, and Welfare on March 14, 1975. Washington, DC: Government Printing Office.
———. 1976. Annual report of the Social Security Administration for fiscal year 1975: Submitted to the Congress by the Department of Health, Education, and Welfare on March 17, 1976. Washington, DC: Government Printing Office.
———. 1977. Annual report of the Social Security Administration for fiscal year 1976: Submitted to the Congress by the Department of Health, Education, and Welfare on April 20, 1977. Washington, DC: Government Printing Office.
Willeford, Carolyn P. 1985. Claims Modernization Project/Field Office Systems Enhancement: An overview. SSA internal document.
Wyatt, Birchard E., and William H. Wandel. 1937. The Social Security Act in operation: A practical guide to the federal and federal-state Social Security programs. Washington, DC: Graphic Arts Press.
Zwintscher, Paula R. 1952. A study of the establishment of the field office of the Bureau of Old-Age and Survivor Insurance: A thesis presented to the graduate council of the faculty of the School of Social Sciences and Public Affairs. Washington, DC: American University.